
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Methods of Examination 3 страница. Renal insufficiency arises in cases where the mass of the active parenchyma is 20 per cent (and lower) of the normal weight
|
|
Renal insufficiency arises in cases where the mass of the active parenchyma is 20 per cent (and lower) of the normal weight. The determination of the mass of the active nephrons is thus important to assess the renal function. The measure of active nephrons is the maximum reabsorption of glucose (normal 300—500 mg/min) and the glomerular filtration rate (normal, 65-120 ml/min).
| UV |
•/ Clearance tests are now widely used to study the renal function according to Van Slyke. Glomerular filtration and tubular reabsorption of water can be measured by clearance tests with substances that are not resorbed or liberated in the tubules. This means that these substances enter urine only by glomerular filtration. Once we assume that a given substance contained in a minute volume of plasma passes entirely into a minute volume of urine, i.e. the plasma is completely cleared of this substance, the filtered amount is then equal to the amount passed with urine. The filtered quantity of substance is equal to the product of glomerular filtration ( F) and its concentration in plasma (P). The quantity excreted with urine is equal to the product of the urine minute volume (V) and the concentration of this substance in the urine (U), i.e, FP = UV. Hence
F =
The U, V, and P values can be found clinically and used for the determination of F that characterizes the volume of plasma which is completely cleared of the given substance during one minute. This volume is called clearance.
If a substance that is filtered in the glomeruli but is not reabsorbed or liberated in the tubules is used for the assessment of renal function, the clearance of this substance is actually equal to glomerular filtration. Using this phenomenon, Rehberg propos ed_a_t est for studying the amoun t, of filtr ation by endogenic or exogenic creatinine.
If one assumes that creatinine content of plasma and glomerular filtrate 's the same, it is possible to determine the degree of concentration of the glomerular filtrate as it passes the tubules. In other words, not only the
Special Part
Chapter 8. Urinary System
I I i
amount of filtration but also of reabsorption can thus be determined (percentage of reabsorbed water):
(F - V) x 100
 .'' F '
.'' F '
In healthy individuals the amount of glomerular filtration is 65—125 ml. The percentage of reabsorbed water is 98.5—99.
''The Rehberg test can be carried out with additional administration of creatinine and liquid, or without it. The second version is used more frequently. Blood is taken from the vein of the patient on a fasting stomach and creatinine concentration is determined. Urine is collected during 2 or 24 hours. Diuresis is measured thoroughly and creatinine content determined. Next, using the formula given above, the amount of glomerular filtration and reabsorption percentage are calculated.
As renal failure develops, glomerular filtration decreases gradually to attain as low values as 5—2—1 ml/min. Tubular reabsorption changes less markedly to decrease in cases of pronounced insufficiency to 80-60 per
cent.
Substances that are not only filtered in the glomeruli but also secreted in the tubules give a mixed clearance, e.g. filtration-reabsorption or filtration-secretion clearance. This clearance is used to assess the renal function in general (rather than its separate function). Clearance of some substances (diodrast, phenol red, para-aminohippuric acid, etc.) is so high that practically approaches the renal blood flow, i.e. the amount of blood that passess the kidneys during one minute. The renal blood flow can thus be determined by the clearance of these substances.
The determination of glomerular filtration is of great clinical significance and is one of the most popular methods for quantitative study of the renal function. The prognostic value of the method increases if it is used in follow-up studies. Thus, persistent decrease in glomerular filtration to 40-50 mg/min during 18-24 months following acute glomerulonephritis suggests the conversion of the acute process into the chronic disease.
X-RAY EXAMINATION
The kidneys are normally not seen on X-ray pictures, except in thin individuals (oval silhouettes can frequently be seen by sides of the spinal column, between the 11th thoracic and 3rd lumbar vertebrae). Stones in the kidneys and the ureters are visualized by X-rays. Best seen are stones containing calcium salts (oxalates and phosphates); stones containing urates are usually not seen. In suspected tumour, X-raying is done after placing

Fig. 104. Pyelograms in norm (a), and in pyelonephritis (b).
pneumoren or pneumoretroperitoneum (administration of oxygen into the retroperitoneal and perirenal space).
Excretory urography is carried out in hospitals: the patient is given intravenously a contrast substance that is readily excreted by the kidneys (25-40 ml of a 30-50 per cent solution of iodine preparation verographin, urotrast, or the like) and then a series of pictures are taken by which determined are the size, position and functional capacity of the kidneys (by the readiness with which they excrete the contrast substance), the size and configuration of the pelves, position of the ureters, and the presence of con-crements (Fig. 104a and b). If the renal function is strongly upset, the contrast substance is poorly excreted, and the procedure fails to give the wanted results. Drop-infusion urography is used for diagnosis of complicated cases. The patient is given 200-250 ml of a 25 per cent solution of a contrast substance by drop infusion during 10—15 minutes. The dose of the infused preparation may be increased with this method while the safety of the procedure is higher since the infusion can immediately be discontinued if first signs of allergic response to the contrast substance appear. The pictures of the kidneys and the ureters obtained by this technique are much better even in decreased renal function. The silhouettes of the
Special Part
Chapter 8. Urinary System

 kidneys are especially well seen on pictures taken immediately after administering the contrast substance. Retrograde pyelography is made for special indications. Liquid contrast substance (urotrast) or gaseous substance (oxygen, air) is administered into the renal pelvis through special ureteral catheter using a cystoscope. Retrograde pyelography is carried out in cases when findings of the excretory pyelography are not reliable or not sufficiently informative to establish correct diagnosis of pelvic affection. Renal angiography (nephroangiography) is used to diagnose disordered blood supply to the kidneys due to upset circulation in the renal artery (stenosis, atherosclerotic plaque, etc.). A special contrast substance (car-diotrast, and the like) is injected into the aorta (through the femoral artery using a special tube) at the level of branching of the renal arteries.
kidneys are especially well seen on pictures taken immediately after administering the contrast substance. Retrograde pyelography is made for special indications. Liquid contrast substance (urotrast) or gaseous substance (oxygen, air) is administered into the renal pelvis through special ureteral catheter using a cystoscope. Retrograde pyelography is carried out in cases when findings of the excretory pyelography are not reliable or not sufficiently informative to establish correct diagnosis of pelvic affection. Renal angiography (nephroangiography) is used to diagnose disordered blood supply to the kidneys due to upset circulation in the renal artery (stenosis, atherosclerotic plaque, etc.). A special contrast substance (car-diotrast, and the like) is injected into the aorta (through the femoral artery using a special tube) at the level of branching of the renal arteries.
CATHETERIZATION OF THE URINARY BLADDER
The urinary bladder is catheterized for both diagnostic and therapeutic purposes (taking urine specimens for studies, evacuation of the accumulated urine from the bladder, in disordered urination, lavage of the bladder with disinfectant solutions, etc.). The urinary bladder is usually catheterized by a soft elastic tube which is sterilized and coated with vaseline oil before use.
CYSTOSCOPY
Cystoscopy is the inspection of the urinary bladder by a cystoscope. The procedure is used to inspect the bladder mucosa, to reveal the presence of ulcers, papilloma, tumours, stones, and also to carry out some therapeutic manipulations. Using a special thin catheter, it is possible to take urine specimens from each kidney and to study the renal function (chromocystoscopy). In chromocystoscopy, the patient is given intravenously 5 ml of a 0.4 per cent indigo carmine solution, and then the time of the appearance of coloured urine from the orifice of the ureter is noted by observation through a cystoscope. In a healthy individual, the urine coloured by indigo carmine begins passing from the ureters in 3-5 minutes following the stain administration. The appearance of the coloured urine from the affected kidney will be delayed, or the urine will not be discharged at all.
KIDNEY BIOPSY
Transcutaneous biopsy of the kidneys is now practised at nephrological departments. A piece of the kidney tissue is taken for histological, histochemical or other examinations by a long needle provided with a syr-
inge (for aspiration). The puncture is made on the side of the loin, over the kidney. In order to reveal the causative agent of pyelonephritis, the obtained sample is cultivated on a nutrient media and the microbial sensitivity to antibiotics is determined. Transcutaneous nephrobiopsy is used to establish the character of the tumour, to diagnose chronic glomerulonephritis, amyloidosis, and in some other cases, but always only for special strict indications, because of the great danger of this procedure.
RADIOGRAPHIC STUDIES
Radioisotope nephrography is used to study the kidney function. The patient is given intravenously diodrast or hippuran labelled with 131I. Then, a multichannel unit is used to determine the rate of blood clearance from the labelled preparation (to show the general secretory function of the kidneys) and accumulation of the preparation in the urinary bladder (to show the general urodynamics in the upper urinary tract).
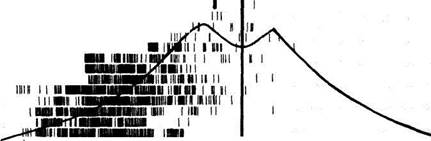
Nephrography is used to study the renal function in chronic glomerulonephritis, tuberculous affection of the kidneys, pyelonephritis, amyloidosis, to diagnose disordered urine outflow from one kidney, and to facilitate differential diagnosis of hypertension (Fig. 105).

|

|
| o o |
| 20 |
| 10 0 |
 Scanning of the kidneys is sometimes used. In this case accumulation of the labelled radioactive preparation (e.g. 203Hg labelled neohydrin) in the kidneys is determined by a special apparatus, gamma-topograph or a scanner. Kidney silhouette is recorded on a paper in the form of a scanogram (Fig. 106). The renal function is assessed by the intensity of accumulation
Scanning of the kidneys is sometimes used. In this case accumulation of the labelled radioactive preparation (e.g. 203Hg labelled neohydrin) in the kidneys is determined by a special apparatus, gamma-topograph or a scanner. Kidney silhouette is recorded on a paper in the form of a scanogram (Fig. 106). The renal function is assessed by the intensity of accumulation

20 10
minutes
pig- 105. Radionephrograms in norm (^4), in chronic glomerulonephritis with upset nitrogen excretory function of the kidneys (B), bilateral hydronephrosis (C), chronic pyelonephritis (a
stone in the left kidney) (D). o—blood clearance; b— radionephrogram of the right kidney; c—radionephrogram of the left kidney.
Special Part
Chapter 8. Urinary System

|
| 1 III I |
| i ii i i nunini ii iinn i II II Illl 1 till 1UI1IIII! I t ii win in ii iiih mi inn i him iiih ii ine imi IN 1 II IHBBI |
| I i i |
| HIMU1I! urn |
| in an mn i in 11 nut i ii i |
i in in
| it in |
II1MM
| I |
i inn nan ii in in
| ii |
| i |
inn iiWHUiHiiiniii. i. imauiiiiiiiMniiiii 11 j in iiiiii iiiiiiiinniiiii ii in him 111 imumi hi
| ti iiii |
| ii ii in i |
urn
mi
Fig. 106. Scanograms. /—normal kidneys; 2— the right kidney affected by hypernephroma.
R
of the preparation (intensity of the silhouette). The presence of focal accumulation defects indicates tumours, cysts, tuberculous affections of the kidneys, and other destructive processes. The shape and size of the kidneys can be determined from a scanogram.
Echography. Echography (ultrasonography) is widely used in nephrology to determine the size and position of the kidneys, the condition of the renal tissue, to reveal cysts, tumours of the parenchyma, stones in the pelves, etc.
Main Clinical Syndromes •
Renal Oedema
Oedem a_Q.f renal aetiology is quite specific in most cases and can easily be differentiated from oedema of other origin, e.g. cardiac oedema, by the affection _of_ loose conn ective_tissue (the eyelids, th e face) r ather than of the lower extremities. Renal oedema Tan develop and resolve quickly. In pronounced cases, oedema is usually uniform over the entire trunk and the extremities (anasarca). Not only the skin but also subcutaneous fat and the internal organs become oedematous. The liver usually becomes oedematous and enlarged, but in renal diseases the enlargement of the liver is usually proportional to enlargement of the other ograns, and is never so pronounced as in cardiac oedema. Greater or lesser amount of fluid is accumulated in the serous cavities, e.g. in the pleural, abdominal, and pericardial cavities. Oedema can be revealed by palpation. It can also be confirmed by the McClure-Aldrich test: 0.2 ml of isotonic sodium chloride solution is injected into the skin on the median surface of a forearm and the time of disappearance of the resulting weal is noted. In a healthy subject, the weal is resolved within one hour. In the presence of a marked oedematous syndrome, the dynamics of oedema during treatment can be better assessed by repeating the test in several days with measurement of girths of the extremities and the abdomen at the same level, by determining the fluid level in the pleural and abdominal cavities, by weighing the patient, and also by determining daily diuresis and water balance of the body (the ratio of the taken and eliminated liquid during 24-hour period).
Oedema, like the general disorder in the water-salt metabolism, arises due to various causes in renal diseases.
1. Diffuse increased permeability of the capillary wall is important in development of oedema in many diseases of the kidneys attended by the oedematous syndrome. Great importance in this process is attributed to auto-immuhe processes and increased hyaluronidase activity of the blood serum, which as a rule, attends many diseases of the kidneys.

|
| 5" £» ff. ft- 2 3 2 P g ft ft K' |
| ft _ 3. 3 Bt o ™ 5 *i o |
Special Part
Chapter 8. Urinary System
 |

|
the blood (due to its intensified reabsorption in the renal tubules) stimulates osmoreceptors and intensifies secretion of the antidiuretic hormone by the pituitary gland, which in turn intensifies the facultative reabsorption of water in distal tubules still more. If the primary cause of oedema (increased capillary permeability, decreased oncotic pressure of plasma) is still active, fluid is not retained in the blood vessels and continues its passage from the blood to the tissues to intensify oedema.
4. Oedema can occur in acute anuria of the kidneys in acute poisoning (e.g. with corrosive sublimate), hypovolaemic reduction of blood circulation in the kidneys (profuse blood loss, shock), and also in the terminal stage of certain chronic renal diseases (retention oedema). But decreased glomerular filtration becomes only important in the presence of other forerunners of oedema rather than an independent factor. For example, in severe renal insufficiency attended by pronounced filtration disturbances, oedema is often absent or even resolved, if any.
It should also be noted that none of the above mechanisms of renal oedema develops independently but becomes only a dominating factor in this or that case.
Nephrotic Syndrome
The nephrotic syndrome (symptom complex) is characterized by pronounced proteinuria, hypoproteinaemia (mainly due to hypoalbumi-naemia), hyperlipidaemia (hypercholesterolaemia), and oedema.
The nephrotic syndrome occurs in chronic glomerulonephritis, amyloidosis, malaria, sepsis, tuberculosis, collagenosis, diabetes mellitus, and certain other diseases. Less frequently the cause of the nephrotic syndrome cannot be established immediately, but in most cases a detailed analysis of anamnestic data and a thorough examination of the patient reveal chronic glomerulonephritis. These forms of the nephrotic syndrome occur mostly in children. Cases where the cause of renal dystrophy is unclear are identified as lipid nephrosis.
It is believed that the nephrotic syndrome is caused by metabolic disorders, mostly upset fat and protein metabolism, with subsequent derangement of trophies and capillary permeability in the glomeruli. Protein and lipids contained in large quantity in primary urine of these patients infiltrate the tubular wall to cause drastic dystrophy in the epithelial cells. The auto-immune mechanism is of great significance for the development of the chronic nephrotic syndrome. It has been proved by animal experiments: small doses of nephrotoxic serum provoke nephritis in rabbits; a picture characteristic of the nephrotic syndrome develops on administration of large doses.
pathological anatomy. The following morphological signs of the nephrotic syndrome develop, in addition to the changes characteristic for the main disease. The kidneys are enlarged (" large white kidneys") and their capsule is easily removed. Histological studies reveal dystrophic changes in the epithelium of the tubules, especially of the convoluted tubules. Lipid deposits can be found in the basal parts of the epithelial cells. The glomeruli are affected by dystrophy; especially specific are changes in podocytes and endothelial cells with which the disordered permeability of the glomerular membrane is associated.
Clinical picture. The main, and often the only complaint of patients is persistent oedema. It is especially pronounced on the face which becomes swollen and pallid, the eyelids are only a narrow slit, and the patient opens his eyes in the morning with difficulty. The legs, the loin, the skin of the abdomen and the hands are also affected by oedema. The oedema is mobile: when the skin is pressed by the finger, a depression remains in it which soon disappears. Fluid is accumulated also in the internal organs and the serous cavities. In typical cases the arterial pressure remains unchanged or even decreased.
As the oedema progresses, diuresis usually decreases and the patient often eliminates only 250-400 ml of urine a day. the specific gravity of the urine is high (1.030-1.040) and it contains much protein, to 10-20 g/1 and more. Cases were reported where the urine contained 24 g/1 of protein. Fine dispersed molecules of albumins prevail among protein. It is believed that the increased filtration of the plasma protein through the glomerular capillary wall and also disordered reabsorption of protein molecules by the affected tubular epithelium are important in the aetiology of proteinuria in the nephrotic syndrome. Great quantity of hyaline, granular and waxy casts, and cells of renal epithelium are found in the urinary sediment. The presence of leucocytes and erythrocytes in the urinary sediment is not characteristic for the nephrotic syndrome. Doubly refracting cholesterol crystals are usually found, which are, as a rule, absent in renal diseases proceeding without the nephrotic syndrome.
A long-standing and persistent proteinuria causes protein depletion of the body and a stable reduction of its content in the blood plasma (1.5 and even 2 times). The albumins become especially deficient, and the albumin to globulin ratio, which is normally 1.2-2.0, decreases significantly. The content of a2-globulins, and also 7-globulins, slightly increases. Proteinuria and hypoproteinaemia (especially hypoalbuminaemia) largely account for oedema that develops in the nephrotic syndrome (see " Renal Oedema"). It has been established that the loss of protein in the urine is aggravated by the renal catabolism of plasma proteins (proteolysis of part of serum protein during its reabsorption in the tubules) and also, probably, by the increased protein loss through the alimentary tract.
Among the constant symptoms are pronounced hyperlipidaemia, in-
33*
Special Part
Chapter 8. Urinary System
 creased blood serum concentration of cholesterol (to 13-15 mmol/1, i.e. 2 or 3 times as great), phospholipids, and neutral fat. These changes are probably secondary to upset protein metabolism and hypoproteinaemia. Laboratory studies reveal three characteristic signs of the nephrotic syndrome: proteinuria, hypoproteinaemia, and upset lipid metabolism (hypercholesterolaemia).
creased blood serum concentration of cholesterol (to 13-15 mmol/1, i.e. 2 or 3 times as great), phospholipids, and neutral fat. These changes are probably secondary to upset protein metabolism and hypoproteinaemia. Laboratory studies reveal three characteristic signs of the nephrotic syndrome: proteinuria, hypoproteinaemia, and upset lipid metabolism (hypercholesterolaemia).
The blood clearing function of the kidneys is not substantially affected in the nephrotic syndrome, and azotaemia does not develop for a Jong time. The main functional renal tests remain normal for a long time, but the tubular secretion can decrease. Biopsy of the kidneys supplies valuable information concerning the nature of the nephrotic syndrome in chronic renal diseases.
Course. If the main disease does not progress, the nephrotic syndrome lasts for years. Oedema and the urinary syndrome intensify at times usually when provoked by an attending infection. Patients with the nephrotic syndrome are sensitive to coccal infection. They often develop recurrent pneumonia and erysipeloid inflammation of the skin. These patients usually died before antibiotics were discovered. Vascular thrombosis is likely to occur in patients with the nephrotic syndrome. The prognosis depends mostly on the main disease and the attending infections.
Treatment. The main disease should be treated. In the presence of pronounced hypoproteinaemia, the patient is prescribed a diet rich in proteins (2-2.5 g/kg body weight without reference to oedema) and poor in sodium chloride. Plasma or concentrated human albumin is given intravenously. Corticosteroids (prednisolone) and immunodepressants (imurane, etc.) are prescribed. If oedema is pronounced, the patient is given diuretics: furan-tril (furocemid), 0.04 g per os every other or third day, in combination with verosperon (0.075-0.15 g/day per os) to remove oedema. Sanatorium and health-resort therapy in dry climate (Central Asia) is recommended during relative remissions.
Renal Hypertension
Renal arterial hypertension is a symptomatic hypertension caused by the affection of the kidneys or renal vessels and upset renal mechanism of arterial pressure regulation. Among all cases of arterial hypertension, renal hypertension makes about 10-15 per cent.
Many diseases of the kidneys, in the first instance acute and chronic glomerulonephritis, pyelonephritis, nephrosclerosis and various affections of the renal blood vessels are attended by elevated arterial pressure. This is underlain by the important role that the kidneys play in the regulation of arterial pressure. The juxtaglomerular apparatus of the kidneys, which is
an accumulation of special cells at the vascular pole of the glomerulus at the point where the artery nears the proximal end of the distal convoluted tubule, produces renin in the presence of ischaemia of the renal parenchyma. Renin acts on the liver-produced hypertensinogen, which is a fraction of a2-globulin of plasma, to convert it into angiotensinogen. The latter is converted enzymatically into angiotensin (hypertensin). Angiotensin stimulates hypersecretion of aldosterone, stenosis of arterioles, and increases arterial pressure. The current literature contains reports on the development of renal hypertension which is associated with renal hyposecretion of special hypotensive substances (e.g. prostaglandins).
It should be noted that due to diffuse spasm of arterioles, essential hypertension also provides conditions for atherosclerosis of the arteries, disordered blood supply to various organs, the kidneys included, and hence for the increased secretion of renin (see " Essential Hypertension"). Therefore, at a certain stage of essential hypertension, further elevation of pressure in the arteries depends largely on the renal mechanism. As distinct from hypertension of other genesis, renal hypertension often tends to run an especially rapid and malignant course (in about 20 per cent of cases).
Like any other hypertension, renal hypertension is manifested by some annoying subjective symptoms, such as headache, dizziness, and noise in the ears (see " Essential Hypertension"). Headache is especially severe in marked elevation of the arterial pressure. It is often attended by vomiting, and paraesthesia. As a rule, the work capacity is impaired and sleep deranged. The increased arterial pressure can be determined by feeling the pulse which appears to be tense. More accurately arterial pressure should be measured instrumentally. Both systolic and diastolic pressure should be measured; the latter pressure is sometimes very high. The second sound is usually accentuated over the aorta.
High and persistent hypertension affects the heart. First, the left-ventricular muscle is hypertrophied due to constant overload. This can be determined by the increased apex beat, specific changes detectable by X-rays (rounded heart apex) and electrocardiographically (deviation of the heart's electrical axis to the left, a certain increase in the/?, wave, and later descent of the S-Tl segment below the zero line, and the negative or two-phase 7\ 2 wave).
At later stages, dystrophic changes occur in the myocardium because its vascularization lags behind the growth of the muscle weight to account for the deficient blood supply; next, cardiosclerosis develops. At the same time, atherosclerosis of the coronary vessels may develop due to upset lipid metabolism, which is characteristic for arterial hypertension and many other renal diseases attended by the nephrotic syndrome. The coronary disease impairs blood supply to the myocardium to an even greater extent.
Special Part
Chapter 8. Urinary System
 | |||
 | |||

|
 Heart pain, like that of angina pectoris often occurs. Further progress of renal diseases can provoke circulatory insufficiency.
Heart pain, like that of angina pectoris often occurs. Further progress of renal diseases can provoke circulatory insufficiency.
Certain acute diseases of the kidneys attended by a rapid and pronounced elevation of the arterial pressure, mainly acute glomerulonephritis, are attended by the condition at which the left ventricle is not hypertrophied enough to compensate for the markedly increased load. Acute ventricular failure can therefore develop. It is manifested by attacks of cardiac asthma and even by a lung oedema.