
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Inquiry 1 страница
|
|
Complaints. The main complaints typical for the respiratory system are dyspnoea, cough, bloody expectorations, and pain in the chest. Fever, asthenia, indisposition and loss of appetite are not infrequent.
Dyspnoea in its manifestation can be subjective, objective, or subjective and objective simultaneously. By subjective dyspnoea is understood the subjective feeling of difficult or laboured breathing. Objective dyspnoea is determined by objective examination and is characterized by changes in the respiration rate, depth, or rhythm, and also the duration of the inspiration or expiration. Diseases of the respiratory system are often accompanied by mixed (i.e. subjective and objective) dyspnoea. It is often associated with rapid breathing (tachypnoea). These symptoms occur in pneumonia, bronchogenic cancer, and in tuberculosis. Cases with purely subjective dyspnoea (in hysteria, thoracic radiculitis) or purely objective dyspnoea (in pulmonary emphysema or pleural obliteration) occur less frequently. Dyspnoea is possible with both normal and slow rate of breathing (bradypnoea). Three types of dyspnoea are differentiated by the prevalent breathing phase: inspiratory dyspnoea, expiratory dyspnoea and mixed dyspnoea when both expiration and inspiration become difficult.
Dyspnoea may be physiological (caused by heavy exercise) and pathological (associated with pathology of the respiratory organs, diseases of the cardiovascular and haemopoietic systems, and poisoning).
Dyspnoea associated with respiratory pathology may be of various aetiology. It can be caused by obstruction of the respiratory ducts, contraction of the respiratory surface of the lungs due to their compression by liquid or air accumulated in the pleural cavity, decreased pneumatization of the lung in pneumonia, atelectasis, infarction or decreased elasticity of the lungs. These conditions are associated with decreased total (vital) lung capacity and ventilation, which causes increased carbon dioxide content of blood, and acidosis of tissues due to accumulation in them of incompletely oxidized metabolites (lactic acid, etc.). The so-called alveolar-capillary block is also possible in some cases. This is associated with exudative and
Special Part
Chapter 5. Respiratory System
proliferative inflammation of the interstitial tissue in interstitial pneumonia or lung oedema.
A mechanical obstruction in the upper respiratory ducts (larynx trachea) complicates and slows down passage of the air into the alveoli and causes inspiratory dyspnoea. When the trachea and a large bronchus are sharply contracted, both inspiration and expiration become difficult and noisy (stridulous respiration). Narrowed lumen in the fine bronchi and bronchioles due to inflammatory oedema and swelling of their mucosa, or else in spasms in the smooth muscles (bronchial asthma), interferes with normal air passage from the alveoli and the expiration becomes difficult. Expiratory dyspnoea thus develops. Pathological conditions caused by a significant decrease in the respiratory surface of the lungs are accompanied by mixed dyspnoea (transient or permanent). Respiration becomes superficial and painful in inflammation of the pleura. Pronounced mixed dyspnoea, often painful, with deep inspiration and expiration occurs in embolism or thrombosis of the pulmonary artery. The patient has to assume a forced, sometimes sitting posture (orthopnoea) to remove the discomfort. Heavy dyspnoea, often followed by asphyxia, is called suffocation. It occurs also in acute oedema of the lungs, bronchiolitis in children, and in fibrinous bronchitis. Asphyxia arising as a sudden attack is asthma. Bronchial asthma, in which an attack of dyspnoea occurs as a result of spasms of smaller bronchi and is accompanied by difficult, lengthy and noisy expiration, is differentiated from cardiac asthma which is secondary to left heart failure and is often accompanied by lung oedema with very difficult expiration.
Cough is a complicated reflex act which is actually a defence reaction aimed at clearing the larynx, trachea, or bronchi from mucus or foreign material. Mucus and inhaled dust particles are normally discharged from the bronchi by ciliated epithelium. But an inflamed bronchial mucosa produces a secretion which acts on the sensitive reflexogenic zones in the respiratory mucosa to stimulate the nerve endings and to activate the coughing reflex. The most sensitive reflexogenic zones are located at branching points of the bronchi, in the tracheal bifurcation points, and in the interarythenoid space of the larynx. The reflexogenic zones producing cough are found in other regions as well, e.g. in the mucosa of the nose, fauces, pleura, etc.
Various diseases of the respiratory organs are characterized by specific cough. The physician should therefore ask the patient to describe the character of his cough, length and time of coughing attacks, loudness and timbre of cough, etc.
Cough may be dry, without sputum, and moist, during which various amounts of sputum of different quality are expectorated. Some diseases
are attended only by dry cough, e.g. laryngitis, dry pleurisy or compression f the main bronchi by the bifurcation lymph nodes (tuberculosis, lym-nhogranulomatosis, cancer metastases, etc.). Bronchitis, pulmonary tuberculosis, pneumosclerosis, abscess, or bronchogenic cancer of the lungs can be first attended by dry cough, which will then turn into moist one with expectoration of the sputum.
If a patient complains of cough with sputum, the physician should try to determine the amount of sputum expectorated during one fit and during the entire day; it is also important to know the time of the day during which the sputum is expectorated and the position of the body at which cough is provoked; the colour, odour, and other properties of sputum are also important. Morning cough is characteristic of patients with chronic bronchitis, bronchiectasis, lung abscess, and cavernous tuberculosis of the lungs. The sputum accumulates during the night sleep in the lungs and the bronchi, but as the patient gets up, the sputum moves to the neighbouring parts of the bronchi to stimulate the reflexogenic zones of the bronchial mucosa. This causes cough and expectoration of the sputum. The amount of the sputum expectorated during the morning may amount to two thirds of the entire daily expectoration. Depending on the gravity of the inflammatory process in patients with mentioned diseases, the daily amount of the expectorated sputum may vary from 10-15 ml to as much as 2 litres. In unilateral bronchiectasis, sputum may be better expectorated in a definite posture, for example, on the right side with bronchiectasis in the left lung, and vice versa. If bronchiectasis is found in the anterior region of the lungs, expectoration is easier in the supine position, and if in the posterior parts, in the prone position.
Patients with pneumonia and bronchitis may complain of cough attacks during the entire day, but attacks may intensify by night (" evening" cough). " Night" cough is characteristic of tuberculosis, lym-Phogranulomatosis, or malignant newgrowths. Enlarged mediastinal lymph nodes in these diseases stimulate the reflexogenic zone of the bifurcation, especially during night when the tone of the vagus nerve increases, to produce the coughing reflex.
Cough is differentiated by its length. It may be permanent and periodic. Permanent cough is rarer and occurs in laryngitis, bronchitis, bronchogenic cancer of the lungs or metastases into the mediastinal lymph nodes, and in certain forms of pulmonary tuberculosis. Periodic cough occurs more frequently. It always occurs in influenza, acute catarrhs of the uPPer air ways, pneumonia, pulmonary tuberculosis, chronic bronchitis, Specially during exacerbation. Periodic cough can be in the form of slight ngie cough bursts (during the initial stage of tuberculosis, in neurosis), Uccession of such bursts, and finally strong and sometimes prolonged at-
S-1SS6
Special Part
Chapter 5. Respiratory System
tacks of cough (in rupture of the abscess, in whooping cough, or when foreign bodies get in the upper air ways). Strong and long cough expulsions sharply increase the intrathoracic pressure and sometimes cause transient dilation of the neck veins, cyanosis, and puffiness of the face. Strong and long fits of cough in children with whooping cough stimulate the adjacent vomiting centre to cause vomiting.
Cough is also classified by its loudness and timbre. Loud barking cough is characteristic of whooping cough, compressed trachea (due to retroster-nal goitre or tumour), affection of the larynx and swelling of the false vocal cords, and in hysteria; soft cough or tussiculation (hacking cough) is characteristic of the first stage of acute lobar pneumonia, dry pleurisy and the early stage of pulmonary tuberculosis. Inflammation of the vocal cords is attended by strong cough while ulceration of the cords is characterized by voiceless cough.
Haemoptysis is expectoration of blood with sputum during cough. The physician must determine the origin of haemoptysis and the amount and character of blood expectorated with sputum. Haemoptysis can develop in diseases of the lungs and air ways (bronchi, trachea or larynx), as well as in diseases of the cardiovascular system. Pulmonary tuberculosis and cancer, virus pneumonia, bronchiectasis, abscess and gangrene of the lung, ac-tinomycosis, tracheitis and laryngitis associated with virus influenza are often attended by haemoptysis. This symptom is also characteristic of some heart defects, such as stenosis of the left venous (mitral) orifice which causes congestion of blood in the lesser circulation, thrombosis or embolism of the pulmonary arteries and subsequent pulmonary infarction.
The amount of blood expectorated with sputum is mostly scant. Blood appears in the form of thin streaks, or it may give diffuse colouration to the sputum, which can be jelly-like or foamy. Cavernous tuberculosis, bronchiectases, degrading tumour and pulmonary infarction may be attended by lung haemorrhage, which is usually accompanied with strong cough.
Blood expectorated with sputum can be fresh and scarlet, or altered. Scarlet blood in the sputum is characteristic of pulmonary tuberculosis, bronchogenic cancer, bronchiectasis, and actinomycosis of the lungs. Blood expectorated with sputum in acute lobar pneumonia (second stage) has the colour of rust (rusty sputum) due to decomposition of the red blood cells and formation of the pigment haemosiderin. Blood in the sputum is fresh and scarlet during the first 2-3 days in lung infarction while in subsequent 7-10 days it becomes altered.
Pain in the chest is classified by its location, origin, character, intensity, duration, and irradiation, by its connection with the respiratory movements, cough, and the posture. Pain may arise during the develop'
nt of a pathological condition in the thoracic wall, the pleura, heart, and the aorta, and in diseases of the abdominal organs (by irradiation). Special linical signs are characteristic of pain of any particular origin, and in this respect pain may have diagnostic value.
pain in the chest wall (" surface" pain) is usually localized, boring or piercing, often intense and prolonged; it intensifies during deep breathing, coughing, lying on the affected side, and in brisk movements. Pain may develop in injury to the skin (trauma, erysipelas, herpes zoster, etc.), muscles (trauma, myositis), intervertebral nerves (thoracic radiculitis in spondylarthrosis), ribs and costal pleura (metastases of the tumour, fractured bones, periostitis).
Pain in the chest in diseases of the respiratory organs depends on irritation of the pleura, especially of the costal and diaphragmal parts where sensitive nerve endings are found. (They are absent in the pulmonary tissue.) Pleura may be injured during its inflammation (dry pleurisy), in subpleural pneumonia (acute lobar pneumonia, lung abscess, pulmonary tuberculosis), in lung infarction, tumour metastasis into the pleura or development in it of the primary tumour, in injury (spontaneous pneumothorax, wound, rib fracture), in subdiaphragmal abscess, and in acute pancreatitis.
Localization of pain depends on the pathological focus. Pain in the left or right inferior part of the chest (pain in the side) is characteristic of dry pleurisy. Inflammation of the diaphragmal pleura may be manifested by pain in the abdomen to simulate acute cholecystitis, pancreatitis, or appendicitis.
Pleural pain is often piercing, while in diaphragmal pleurisy and spontaneous pneumothorax it is acute and intense. Pain is intensified in deep breathing, coughing, or when the patient lies on the healthy side. The respiration movements in this position become more intense in the affected side of the chest to strengthen friction of the inflamed pleura (rough from deposited fibrin). Pain lessens when the patient lies on the affected side. Pleural pain is also lessened when the chest is compressed to decrease the respiratory excursions.
Pain in cardiovascular diseases is localized in the region of the heart or the retrosternal region. It arises in physical strain, excitement, and unfavourable emotions. The attack often develops suddenly and may continue from a few seconds to several hours. Pressing pain of various intensity often occurs as the feeling of discomfort in the chest. Neurosis of the heart is manifested by intermittent cutting pain at the apex of the heart. pain intensity does not change during cough, deep breathing or movements 01 the body. Tumour of the mediastinum may be attended by permanent
ense retrosternal pain which is sometimes attended by signs of compres-
Special Part
Chapter 5. Respiratory System
sion of large mediastinal vessels. Retrosternal pain may arise in hiatus hernia or by reflectory routes in case of ulcer, tumour of the cardiac part of the stomach, and in cholelithiasis.
Anamnesis. When questioning the patient the physician should determine the time the disease began. Acute onset is characteristic of acute pneumonia, especially acute lobar pneumonia. Pleurisy begins more gradually. A non-manifest onset and a prolonged course are characteristic of pulmonary tuberculosis and cancer. The onset of many diseases may be provoked by chills (bronchitis, pleurisy, pneumonia).
Determining epidemiological conditions is very important for establishing the cause of the disease. Thus influenzal pneumonia often occurs during epidemic outbreaks of influenza. Establishing contacts with tuberculosis patients is also very important. Specific features of the course of the disease and the therapy given (and its efficacy) should then be established.
When collecting the life anamnesis, the physician should pay attention to conditions under which the patient lives and works. Damp premises with inadequate ventilation or work in the open (builders, truck drivers, agricultural workers, etc.) can become the cause of acute inflammation of the lungs with more frequent conversion into chronic diseases. Some dusts are harmful and cause bronchial asthma. Coal dust causes a chronic disease of the lungs called anthracosis. Regular exposure to silica dust (cements, pottery, etc.) causes silicosis, the occupational fibrosis of the lungs.
The patient should give a detailed report of his past diseases of the lungs or pleura, which helps the physician establish connections between the present disease and diseases of the past history.
Physical Examination
INSPECTION
Examination of the chest should be done according to a definite plan. The general configuration of the chest should firet be estimated (position of the clavicles, supra- and subclavicular fossae, shoulder blades); the next step is to define the type, rhythm and frequency of breathing, respiratory movements of the left and right shoulder blades, and of the shoulder girdle, and involvement of the accessory respiratory muscles in the breathing act. The patient should be better examined in the upright (standing or sitting) position with the chest being naked. Illumination of the body should be uniform.
The shape of the chest may be normal or pathological. A normal chest is characteristic of healthy persons with regular body built. Its right and
left sides are symmetrical, the clavicles and the shoulder blades should be at one level and the supraclavicular fossae equally pronounced on both sides. Since all people with normal constitution are conventionally divided into three types, the chest has different shape in accordance with its constitutional type. Pathological shape of the chest may be the result of congenital bone defects and of various chronic diseases (emphysema of the lungs, rickets, tuberculosis).
Normal form of the chest. 1. Normosthenic (conical) chest in subjects with normosthenic constitution resembles a truncated cone whose bottom is formed by well-developed muscles of the shoulder girdle and is directed upward. The anteroposterior (sternovertebral) diameter of the chest is smaller than the lateral (transverse) one, and the supraclavicular fossae are slightly pronounced. There is a distinct angle between the sternum and the manubrium (angulus Ludowici); the epigastric angle nears 90°. The ribs are moderately inclined as viewed from the side; the shoulder blades closely fit to the chest and are at the same level; the chest is about the same height as the abdominal part of the trunk.
2. Hypersthenic chest in persons with hypersthenic constitution has the
shape of a cylinder. The anteroposterior diameter is about the same as the
transverse one; the supraclavicular fossae are absent (level with the chest).
The manubriosternal angle is indistinct; the epigastric angle exceeds 90°;
the ribs in the lateral parts of the chest are nearly horizontal, the intercostal
space is narrow, the shoulder blades closely fit to the chest, the thoracic
part of the trunk is smaller than the abdominal one.
3. Asthenic chest in persons with asthenic constitution is elongated,
narrow (both the anteroposterior and transverse diameters are smaller than
normal); the chest is flat. The supra- and subclavicular fossae are distinctly
pronounced. There is no angle between the sternum and the manubrium:
the sternal bone and the manubrium make a straight " plate". The
epigastric angle is less than 90°. The ribs are more vertical at the sides, the
tenth ribs are not attached to the costal arch (costa decima fluctuens); the
intercostal spaces are wide, the shoulder blades are winged (separated from
the chest), the muscles of the shoulder girdle are underdeveloped, the
shoulders are sloping, the chest is longer than the abdominal part of the
trunk.
Pathological chest. 1. Emphysematous {barrel-like) chest resembles a hypersthenic chest in its shape, but differs from it by a barrel-like conjuration, prominence of the chest wall, especially in the posterolateral regions, the intercostal spaces are enlarged. This type of chest is found in chronic emphysema of the lungs, during which elasticity of the lungs decreases while the volume of the lungs increases; the lungs seem to be as if at the inspiration phase. Natural expiration is therefore difficult not only
Special Part
Chapter 5. Respiratory System
during movements but also at rest (expiratory dyspnoea is found). Active participation of accessory respiratory muscles in the respiratory act (especially m. sternocleidomastoideus and m. trapezius), depression of the intercostal space, elevation of the entire chest during inspiration and relaxation of the respiratory muscles and lowering of the chest to the initial position during expiration become evident during examination of emphysema patients.
2. Paralytic chest resembles the asthenic chest. It is found in emaciated patients, in general asthenia and constitutional underdevelopment; it often occurs in grave chronic diseases, more commonly in pulmonary tuberculosis and pneumosclerosis, in which fibrous tissue contracts the lungs and diminishes their weight due to the progressive chronic inflammation. During examination of patients with paralytic chest, marked atrophy of the chest muscles and asymmetry of the clavicles and dissimilar depression of the supraclavicular fossae can be observed along with typical signs of asthenic chest. The shoulder blades are not at one level either, and their movements during breathing are asynchronous.
3. Rachitic chest {keeled or pigeon chest). It is characterized by a markedly greater anteroposterior diameter (compared with the transverse diameter) due to the prominence of the sternum (which resembles the keel of a boat.) The anterolateral surfaces of the chest are as if pressed on both sides and therefore the ribs meet at. an acute angle at the sternal bone, while the costal cartilages thicken like beads at points of their transition to bones (rachitic beads). As a rule, these beads can be palpated after rickets only in children and youths.
4. Funnel chest can occur in normosthenic, hypersthenic or asthenic
subjects; it has a funnel-shaped depression in the lower part of the ster
num. This deformity can be regarded as a result of abnormal development
of the sternum or prolonged compressing effect. In older times this chest
would be found in shoemaker adolescents. The mechanism of formation of
the funnel chest was explained by the permanent pressure of the chest
against the shoe; the funnel chest was therefore formerly called cobbler
chest.
5. Foveated chest is almost the same as the funnel chest except that the
depression is found mostly in the upper and the middle parts of the anterior
surface of the chest. This abnormality occurs in syringomyelia, a rare
disease of the spinal cord.
The chest may be abnormal in subjects with various deformities of the spine which arise as a result of injuries, tuberculosis of the spine, rheumatoid arthritis (Bekhterev's disease), etc. Four types of spine deformities are distinguished: (1) lateral curvature of the spine, called scoliosis; (2) excessive forward and backward curvature of the spine (gibbus and
wphosis, respectively); (3) forward curvature of the spine, generally in the mbar region (lordosis); (4) combination of the lateral and forward curvature of the spine (kyphoscoliosis).
Scoliosis is the most frequently occurring deformity of the spine. It mostly develops in schoolchildren due to bad habitual posture. Kyphoscoliosis occurs less frequently. Lordosis only occurs in rare cases. Curvature of the spine, especially kyphosis, lordosis, and kyphoscoliosis cause marked deformation of the chest to change the physiological position of the lungs and the heart and thus interfere with their normal functioning.
The shape of the chest can readily change due to enlargement or diminution of one half of the chest (asymmetry of the chest). These changes can be transient or permanent.
The enlargement of the volume of one half of the chest can be due to escape of considerable amounts of fluid as the result of inflammation (ex-udate) or non-inflammatory fluid (transudate) into the pleural cavity, or due to penetration of air inside the chest in injuries (pneumothorax). Levelling or protrusion of the intercostal spaces, asymmetry of the clavicles and the shoulder blades and also unilateral thoracic lagging can be observed during examination of the enlarged part of the chest. The chest assumes normal shape after the air or fluid is removed from the pleural cavity.
One part of the chest may diminish due to (1) pleural adhesion or complete closure of the pleural slit after resorption of effusion (after prolonged presence of the fluid in the pleural cavity); (2) contraction of a considerable portion of the lung due to growth of connective tissue (pneumosclerosis) after acute or chronic inflammatory processes, such as acute lobar pneumonia (with subsequent carnification of the lung), lung infarction, pulmonary abscess, tuberculosis, etc.; (3) resection of a part or the entire lung; (4) atelectasis (collapse of the lung or its portion) that may occur due to closure of the lumen in a large bronchus by a foreign body or a tumour growing into the lumen of the bronchus and causing its obturation. The closure of the air passage into the lung with subsequent resorption of air from the alveoli and a decrease in the volume of the lung diminish the corresponding half of the chest. The chest thus becomes asymmetrical, the shoulder of the affected side lowers, the clavicle and the scapula lower as *ell, and their movements during deep respiration become slower and lrnited; the supra- and subclavicular fossae become more depressed, the in-ercostal spaces decrease in size or become invisible. The marked depres-^°n of the supraclavicular fossa on one side often depends on the diminu-" °n of the apex of a fibrosis-affected lung.
Respiratory movements of the chest should be examined during inspec-
n of the patient. In physiological conditions they are performed by the
Special Part
Chapter 5. Respiratory System
contraction of the main respiratory muscles: intercostal muscles, muscl of the diaphragm, and partly the abdominal wall muscles. The so-called a& cessory respiratory muscles (mm. sternocleidomastoideus, trapezius PeC" toralis major et minor, etc.) are actively involved in the respirator0* movements in pathological conditions associated with difficult breathing
The type, frequency, depth and rhythm of respiration can be deter mined by carefully observing the chest and the abdomen. Respiration can be costal (thoracic), abdominal, or mixed type.
Thoracic (costal) respiration (Fig. 10o). Respiratory movements are carried out mainly by the contraction of the intercostal muscles. The chest markedly broadens and slightly rises during inspiration, while during ex piration it narrows and slightly lowers. This type of breathing is known as costal and is mostly characteristic of women.
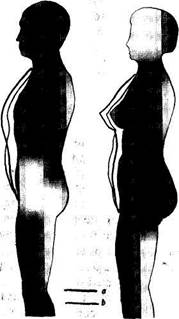 Abdominal respiration. Breathing is mainly accomplished by the diaphragmatic muscles; during the inspiration phase the diaphragm contracts and lowers to increase rarefaction in the chest and to suck in air into the lungs. The intra-abdominal pressure increases accordingly to displace anteriorly the abdominal wall. During expiration the muscles are relaxed, the diaphragm rises, and the abdominal wall returns to the initial position! This type of respiration is also called diaphragmatic (Fig. 106) and is mostly characteristic of men.
Abdominal respiration. Breathing is mainly accomplished by the diaphragmatic muscles; during the inspiration phase the diaphragm contracts and lowers to increase rarefaction in the chest and to suck in air into the lungs. The intra-abdominal pressure increases accordingly to displace anteriorly the abdominal wall. During expiration the muscles are relaxed, the diaphragm rises, and the abdominal wall returns to the initial position! This type of respiration is also called diaphragmatic (Fig. 106) and is mostly characteristic of men.
Fig. 10. Types of respiration. a —thoracic; b —abdominal.
Mixed respiration. The respiratory movements are carried out •rnultaneously by the diaphragm and the intercostal muscles. In nhysiological conditions this respiration sometimes occurs in aged persons Ld in some pathological conditions of the respiratory apparatus and the abdominal viscera. For example, in women with dry pleurisy, pleural adhesion, myositis, and thoracic radiculitis, the contractile activity of the intercostal muscles decreases and the respiratory movements are carried out by the accessory movements of the diaphragm. In extensive pleural adhesion, lung emphysema, and in strong pain in the chest due to acute inflammation of the intercostal muscles or nerves, respiration is temporarily carried out by the diaphragmatic muscles exclusively. Mixed respiration occurs in men with underdeveloped diaphragmatic muscles, in diaphragmatitis, acute cholecystitis, perforating ulcer of the stomach or the duodenum. Respiration in such cases is sometimes carried out only by the intercostal muscles.
Respiration rate. Respiration rate can be determined " by counting the movements of the chest or the abdominal wall, with the patient being unaware of the procedure. The pulse rate should first be taken and then the respiration rate. The number of respiratory movements in a healthy adult at rest should be 16 to 20 per minute, in the newborn 40-45, this rate gradually decreasing with age. The respiration rate decreases during sleep to 12-14 per minute, while under physical load, emotional excitement, or after heavy meals the respiration rate increases.
The respiration rate alters markedly in some pathological conditions. The causes of accelerated respiration may be (1) narrowing of the lumen of small bronchi due to spasms or diffuse inflammation of their mucosa (bronchiolitis occurring mostly in children), which interfere with normal passage of air into the alveoli; (2) decreased respiratory surface of the lungs due to their inflammation and tuberculosis, in collapse or atelectasis of the lung due to its compression (pleurisy with effusion, hydrothorax, pneumothorax, tumour of mediastinum), in obturation or compression of the main bronchus by a tumour, in thrombosis or embolism of the pulmonary artery, in pronounced emphysema, when the lung is overfilled with blood or in a case of lung oedema in certain cardiovascular diseases; (3) insufficient depth of breathing (superficial respiration) which can be due to difficult contractions of the intercostal muscles or the diaphragm in acute pain (dry pleurisy, acute myositis, intercostal neuralgia, rib fracture, Or tumour metastasis into the ribs), in a sharp increase in the intra-abdominal pressure and high diaphragm (ascites, meteorism, late pregnan-cv), and finally in hysteria.