
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Inquiry 3 страница
|
|
Special Part
Chapter 5. Respiratory System
 | |
 |

|
|

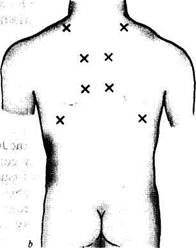
Fig. 18. Lung listening points.
., anterior (a) and posterior (b) surface of the chest.
Respiratory murmurs (breath sounds) during various phases of respiration are first compared during auscultation of the lungs as well as their character, length, and intensity (loudness). Then these sounds are compared with the respiratory murmurs at the symmetrical points of the other half of the chest (comparative auscultation). Attention should be paid to the main respiratory sounds, such as vesicular (alveolar) breathing which is heard over the pulmonary tissues, and bronchial (laryngotracheal) breathing which is heard over the larynx, trachea, and large bronchi.
In the presence of pathology in the air ways, in the alveolar tissue or in the pleura, adventitious sounds such as rales, crepitation, and pleural friction, are heard in addition to the main breath sounds during inspiration and expiration. These adventitious sounds should be examined only after the character of the main sounds has been established. Normal breathing sounds should be better auscultated with the nasal breathing (with the patient's mouth closed) while adventitious sounds are better heard with deep respiration through the open mouth.
Vesicular breathing. Respiratory sounds known as vesicular breathing arise due to vibration of the elastic elements of the alveolar walls during their filling with air in inspiration. The alveoli are filled with air in sequence. Therefore, the summation of the great number of sounds produced during vibration of the alveolar walls gives a long soft (blowing) noise that can be heard during the entire inspiration phase, its intensity
radually increasing. This sound can be simulated by pronouncing the 8ound 'f during inspiration, or by drawing tea from a saucer. Alveolar walls still vibrate at the initial expiration phase to give a shorter second phase of the vesicular breathing, which is heard only during the first third of the expiration phase (Fig. 19c), because vibrations of elastic alveolar walls are quickly dampened by the decreasing tension of the alveolar walls.
Normal vesicular breathing is better heard over the anterior surface of the chest, below the 2nd rib, laterally of the parasternal line, and also in the axillary regions and below the scapular angle, i.e. at points where the largest masses of the pulmonary tissue are located. Vesicular breathing is heard worse at the apices of the lungs and their lowermost parts, where the masses of the pulmonary tissue are less abundant. While carrying out comparative auscultation, it should be remembered that the expiration sounds are louder and longer in the right lung due to a better conduction of the laryngeal sounds by the right main bronchus, which is shorter and wider. The respiratory sound sometimes becomes bronchovesicular over the right apex; or it may be mixed due to more superficial and horizontal position of the right apical bronchus.
Alterations in vesicular breathing. Vesicular breathing can vary, i.e. it may be louder or softer for both physiological and pathological reasons.
Physiological weakening of vesicular breathing (Fig. 196) occurs in patients with thicker chest wall due to excessively developed muscles or subcutaneous fat. Physiological intensification of vesicular breathing (Fig. 19c) may be observed in patients with underdeveloped muscles or subcutaneous fat. Intensified vesicular breathing is characteristic of children with a thin chest wall, good elasticity of the alveoli and the in-

|
Fig. 19. Types of respiration.
a —vesicular; b —decreased vesicular; c —increased vesicular; d —bronchial; e — decreased bronchial; /—increased bronchial; g—bronchovesicular; h —cogwheel.
Special Part
Chapter 5. Respiratory System
teralveolar septa. This respiration is called 'puerile respiration' (L pUe child). Vesicular respiration is intensified during exercise; respiratory movements become deeper and more frequent. Physiological changes in vesicular respiration always involve both parts of the chest, and respiratory sounds are equally intensified or weakened at the symmetrical points of the chest.
In pathology, alterations in vesicular breathing may be both uni- and bilateral, or else only over one lobe of the lung. Respiratory sounds become weaker or inaudible at all; or they may be intensified. Alterations in vesicular respiration in such cases depend on the amount of intact alveoli and the properties of their walls, the amount of air contained in them, on the length and strength of the expiration and inspiration phases, and finally on the conditions of sound conduction from the vibrating elastic elements of the pulmonary tissue to the surface of the chest.
Pathologically decreased vesicular respiration can be due to a significantly diminished number of the alveoli because of atrophy and gradual degradation of the interalveolar septa and formation of larger vesicles incapable of collapsing during expiration. This pathological condition is observed in pulmonary emphysema, at which the remaining alveoli are no longer elastic; their walls become incapable of quick distention and do not give sufficiently strong vibrations.
Decreased vesicular breathing can be due to inflammation and swelling of the walls in a part of the lung and decreased amplitude of their vibration during inspiration, which is characteristic of early acute lobar pneumonia. During the second stage of this disease, the alveoli of the affected part of the lung become filled with effusion and vesicular breathing becomes inaudible over this region. Vesicular breathing can be decreased also in insufficient delivery of air to the alveoli through the air ways because of their mechanical obstruction (e.g. by a tumour). Air admission to the alveoli can be decreased in patients with a markedly weakened inspiration phase (as a result of inflammation of the respiratory muscles, intercostal nerves, rib fracture, extreme asthenia of the patient and adynamia).
Vesicular respiration decreases also due to obstructed conduction of sound waves from the source of vibration (alveolar walls) to the chest surface, as, for example, in thickening of the pleural layers or accumulation of air or fluid in the pleural cavity. If the amount of fluid or air in the pleural cavity is great, respiratory sounds are not heard. Conduction of sound to the surface of the chest may be absent in atelectasis of the lung due to complete obstruction of the lumen in the large bronchus.
Abnormally increased vesicular breathing (Fig. 19c) can be heard during expiration or during both respiratory phases. Increased expiration depends on obstruction to the air passage through small bronchi or their
ontracted lumen (inflammatory oedema of the mucosa, bronchospasm). cxpiration becomes louder and longer.
Deeper vesicular breathing during which the inspiration and expiration ohases are intensified, is called harsh. It occurs in marked and non-uniform narrowing of the lumen in small bronchi and bronchioles due to inflammatory oedema of their mucosa (bronchitis).
Another type of pathological respiration is interrupted or cogwheel respiration. This vesicular respiration is characterized by short jerky inspiration efforts interrupted by short pauses between them; the expiration is usually normal. Interrupted breathing also occurs in non-uniform contraction of the respiratory muscles, e.g. when a patient is auscultated in a cold room, or when he has nervous trembling, or diseases of the respiratory muscles, etc. Interrupted breathing over a limited part of the lung indicates difficult passage of air from small bronchi to the alveoli in this region and uneven unfolding of the alveoli. Interrupted breathing indicates pathology in fine bronchi and is more frequently heard at the apices of the lungs during their tuberculous infiltration.
Bronchial breathing. Respiratory sounds known as bronchial or tubular breathing (Fig. 19c/) arise in the larynx and the trachea as air passes through the vocal slit. As air is inhaled, it passes through the vocal slit to enter wider trachea where it is set in vortex-type motion. Sound waves thus generated propagate along the air column throughout the entire bronchial tree. Sounds generated by the vibration of these waves are harsh. During expiration, air also passes through the vocal slit to enter a wider space of the larynx where it is set in a vortex motion. But since the vocal slit is narrower during expiration, the respiratory sound becomes louder, harsher and longer. This type of breathing is called laryngotracheal (by the site of
its generation).
Bronchial breathing is well heard in physiological cases over the larynx, the trachea, and at points of projection of the tracheal bifurcation (anteriorly, over the manubrium sterni, at the point of its junction with the sternum, and posteriorly in the interscapular space, at the level of the 3rd and 4th thoracic vertebrae). Bronchial breathing is not heard over the other parts of the chest because of large masses of the pulmonary tissue found between the bronchi and the chest wall.
Bronchial breathing can be heard instead of vesicular (or in addition to the vesicular breathing) over the chest in pulmonary pathology. This breathing is called pathological bronchial respiration. It is conducted to the surface of the chest wall only under certain conditions, the main one being mduration of the pulmonary tissue when the alveoli are filled with effusion (acute lobar pneumonia, tuberculosis, etc.), with blood (lung infarction), Or due to compression of the alveoli by air or fluids accumulated in the
Special Part
Chapter 5. Respiratory System
pleural cavity, and compression of the lung against its root (compression atelectasis). In such cases the alveolar walls do not vibrate, while consolidated airless pulmonary tissue becomes a good conductor of sound waves in laryngotracheal respiration to the surface of the chest wall. Lungs may be consolidated due to replacement of the inflated pulmonary tissue by connective tissue (pneumosclerosis, carnification of the lung lobe, which sometimes occurs in acute lobar pneumonia due to growth of connective tissue into the inflamed lobe of the lung, etc.).
Depending on degree of induration, its size and location in the lung, pathological bronchial breathing may have different intensity and pitch. If the induration is large and superficial, loud bronchial breathing is heard. It is heard as if near the ear; the pitch of the sound is higher in this case (Fig. 19/). Bronchial breathing can be heard in acute lobar pneumonia at its second stage (affection of the entire lobe of the lung). If a segment of a lung is indurated, and the affection is deep seated, breathing will be weaker and the pitch lower (Fig. 19e). This sound can be heard in lobular pneumonia if several foci are close to one another or fuse together to form a large focus of induration (confluent pneumonia). Especially soft and low sounds are heard in patients with compression atelectasis. The sound resembles an echo, as if entering the physician's ear from a far off source.
Pathological bronchial respiration can be heard if an empty cavity is formed in the lung (abscess, cavern) and it is communicated with the bronchus. Consolidation of pulmonary tissue round the focus facilitates conduction of sound waves of laryngotracheal breathing to the surface of the chest wall, the more so that the sound is intensified in the resonant cavity and that at the moment of air passage from the narrow bronchus the air is set in a vortex motion.
Amphoric respiration arises in the presence of a smooth-wall cavity (not less than 5—6 cm in diameter) communicated with a large bronchus. Because of a strong resonance, additional high overtones appear along with the main low-pitch laryngotracheal breathing. These overtones alter the main tone of the bronchial respiratory sound. Sounds of this kind can be produced by blowing over the mouth of an empty glass or clay jar. This altered bronchial breathing is therefore called amphoric (Gk amphoreus jar).
Metallic respiration differs from both bronchial and amphoric. It is loud and high, and resembles the sound produced when a piece of metal is struck. Metallic respiration is heard in open pneumothorax when the air of the pleural cavity communicates with the external air.
Stenotic respiration is exaggerated laryngotracheal breathing, which is heard in cases with narrowed trachea or a large bronchus (due to a tumour); it is heard mainly at points where physiological bronchial breathing is normally heard.
gronchovesicular or mixed respiration is heard in lobular pneumonia or • filtrative tuberculosis, and also in pneumosclerosis, with foci of con-1olidated tissue being seated deeply in the pulmonary tissue and far from ne another. Mixed breathing, when the inspiration phase is characteristic of vesicular breathing and the expiration phase of bronchial breathing, is often heard in such cases instead of weak bronchial breathing.
adventitious sounds are rales, crepitation, and pleural friction.
Rales arise in pathology of the trachea, bronchi, or if a cavern is formed in the affected lung. Rales are classified as dry (rhonchi) and moist rales.
Dry rales, or rhonchi, may be due to various causes. The main one is constriction of the lumen in the bronchi. Constriction may be total (in bronchial asthma), non-uniform (in bronchitis), or focal (in tuberculosis or tumour of the bronchus). Dry rales can be due to (1) spasms of smooth muscles of the bronchi during fits of bronchial asthma; (2) swelling of the bronchial mucosa during its inflammation; (3) accumulation of viscous sputum in the bronchi which adheres to the wall of the bronchus and narrows its lumen; (4) formation of fibrous tissue in the walls of separate bronchi and in the pulmonary tissue with subsequent alteration of their architectonics (bronchiectasis, pneumosclerosis); (5) vibration of viscous sputum in the lumen of large and medium size bronchi during inspiration and expiration: being viscous, the sputum can be drawn (by the air stream) into threads which adhere to the opposite walls of the bronchi and vibrate
like strings.
Dry rales are heard during inspiration and expiration and vary greatly in their loudness, tone and pitch. According to the quality and pitch of the sounds produced, dry rales are divided into sibilant (high-pitched and whistling sounds) and sonorous rales (low-pitched and sonoring sounds). High-pitched rales are produced when the lumen of the small bronchi is narrowed, while low-pitched sonorous rales are generated in stenosis of medium calibre and large calibre bronchi or when viscous sputum is accumulated in their lumen.
Propagation and loudness of dry rales depend on the size of the affected area in the bronchial tree, on the depth of location of the affected bronchi, and the force of the respiratory movements. When the walls of a medium size and large bronchi are affected to a limited extent, rhonchi are ^significant and soft. Diffuse inflammation of the bronchi or bron-chospastn arising during attacks of bronchial asthma is attended by both mgh-pitched sibilant and low-pitched sonorous rales which vary in tone and loudness. These rhonchi can be heard at a distance during expiration.. fhonchi are due to accumulation of viscous sputum in the bronchi, dur-lng deep breathing (or immediately after coughing) they can be either intended or weakened, or else disappear altogether for a short time.
Special Part
Chapter 5. Respiratory System
Moist rales are generated because of accumulation of liquid secretion (sputum, oedematous fluid, blood) in the bronchi through which air passes. Air bubbles pass through the liquid secretion of the bronchial lumen and collapse to produce the specific cracking sound. This sound can be simulated by bubbling air through water using a fine tube. Moist rales are heard during both the inspiration and expiration, but since the air velocity is higher during inspiration, moist rales will be better heard at this respiratory phase.
Depending on the calibre of bronchi where rales are generated, they are classified as fine, medium and coarse bubbling rales. Fine bubbling rales are generated in fine bronchi and are percepted by the ear as short multiple sounds. Rales originating in the finest bronchi and bronchioles are similar to crepitation from which they should be differentiated (see below). Medium bubbling rales are produced in bronchi of a medium size and coarse bubbling rales in large calibre bronchi, in large bronchiectases, and in pulmonary cavities (abscess, cavern) containing liquid secretions and communicating with the large bronchus. Large bubbling rales are characterized by a lower and louder sound.
Moist rales originating in superficially located large cavities (5—6 cm and over in diameter) may acquire a metallic character. If segmentary bronchiectases or cavities are formed in the lung, rales can usually be heard over a limited area of the chest. Chronic bronchitis or marked congestion in the lungs associated with failure of the left chambers of the heart is as a rule attended by bilateral moist rales of various calibre, which occur at the symmetrical points of the lungs.
. Depending on the character of the pathology in the lungs, moist rales are subdivided into consonating or crackling, and non-consonating or bubbling rales. Consonating moist rales are heard in the presence of liquid secretions in the bronchi surrounded by airless (consolidated) pulmonary tissue or in lung cavities with smooth walls surrounded by consolidated pulmonary tissue. The cavity itself acts as a resonator to intensify moist rales. Moist consonating rales are heard as if just outside the ear. Consonating rales in the lower portions of the lungs suggest inflammation of the pulmonary tissue surrounding the bronchi. Consonating rales heard in the subclavicular or subscapular regions indicate tuberculous infiltration or cavern in the lung.
Non-consonating rales are heard in inflammation of bronchial mucosa (bronchitis) or acute oedema of the lung due to the failure of the left chambers of the heart. The sounds produced by collapsing air bubbles in the bronchi are dampened by the " air cushion" of the lungs as they are conducted to the chest surface.
The so-called falling-drop sound (gutta cadens) can be heard by auscultation. It can occur large cavities of the lungs or at the base of the pleural cavity which contain liquid pus or air the patient changes his posture from recumbent to upright position or vice versa. Tenacious ntaining pus sticks to the surface of the cavity and as the patient changes his position Others in drops which fall one after another into the liquid (sputum or pus) accumulated at the bottom.
Crepitation. As distinct from rales, crepitation originates in the alveoli. Some authors erroneously classify these sounds as crepitant and subcrepi-tant rales. Crepitation is a slight crackling sound that can be imitated by rubbing a lock of hair. The main condition for generation of crepitation is accumulation of a small amount of liquid secretion in the alveoli. During expiration, the alveoli stick together, while during inspiration the alveolar walls are separated with difficulty and only at the end of the inspiratory movement. Crepitation is therefore only heard during the height of inspiration. In other words, crepitation is the sound produced by many alveoli during their simultaneous reinflation.
Crepitation is mainly heard in inflammation of the pulmonary tissue, e.g. at the first (initial) and third (final) stages of acute lobar pneumonia, when the alveoli contain small amounts of inflammatory exudate, in in-filtrative pulmonary tuberculosis, lung infarction, and finally in congestions that develop due to insufficient contractile function of the left-ventricular myocardium or in marked stenosis of the left venous orifice of the heart. Crepitation can be heard in the inferolateral portions of the lungs of aged persons during first deep inspirations, especially so if the patient was in the recumbent position before auscultation. The same temporary crepitation can be heard in compressive atelectasis. During pneumonia, crepitation is heard over longer periods and disappears when a large amount of inflammatory secretion is accumulated in the alveoli or after its complete resolution.
By its acoustic properties, crepitation can often resemble moist fine rales that are produced in fine bronchi or bronchioles filled with liquid secretion. Differentiation of moist rales from crepitation is of great diagnostic importance. Persistent crepitation may indicate pneumonia while fine non-consonating rales suggest bronchitis. Differential-diagnostic signs of these rales and crepitation are as follows: moist fine rales are heard during both inspiration and expiration; they can be intensified or disappear after coughing, while crepitation can only be heard at the height of inspira-toon; nor does it change after coughing.
Pleural friction sound. In physiological conditions visceral and parietal
ayers of the pleura are constantly " lubricated" by a capillary layer of
eural fluid and are therefore smooth. Their friction during breathing is
I
noiseless. Various pathological conditions alter the physical properties of the pleural surfaces and their friction against one another becomes more intense to generate a peculiar adventitious noise, known as the pleural fric. tion sound. Fibrin is deposited in inflamed pleura to make its surface rough; moreover, cicatrices, commissures, and bands are formed between pleural layers at the focus of inflammation. Tuberculosis or cancer are also responsible for the friction sounds.
Pleural friction sounds are heard during both inspiration and expiration. The sounds are differentiated by intensity, or loudness, length, and site over which they are heard. During early dry pleurisy the sounds are soft and can be imitated by rubbing silk or fingers in the close vicinity of the ear. The character of pleural friction sound is altered during the active course of dry pleurisy. It can resemble crepitation or fine bubbling rales (sometimes crackling of snow). In pleurisy with effusion, during the period of rapid resorption of exudate, the friction sound becomes coarser due to massive deposits on the pleural surfaces. This friction (to be more exact, vibrations of the chest) can be even identified by palpation of the chest.
The time during which pleural friction sound can be heard varies with diseases. For example, in rheumatic pleurisy pleural friction is only heard during a few hours; after a period of quiescence it reappears. Pleural friction persists for a week and over in dry pleurisy of tuberculous aetiology and pleurisy with effusion at the stage of resorption. Pleural friction sounds can be heard in some patients for years after pleurisy because of large cicatrices and roughness of the pleural surfaces.
The point over which pleural friction can be heard depends on the focus of inflammation. Most frequently it is heard in the inferolateral parts of the chest, where the lungs are most mobile during respiration. In rare cases this sound can be heard over the lung apices, when they are affected by tuberculosis with involvement of the pleural membranes.
If the inflammatory focus is localized in the pleura adjacent to the heart, pleuropericardial friction sound may be heard during both inspiration and expiration, and also during cardiac systole and diastole. As distinct from cardiac murmurs, this noise is best heard at the height of a deep inspiration because at that time the pleural surfaces come in closer contact with the pericardium.
Pleural friction sounds can be differentiated from fine bubbling rales and crepitation by the following signs: (1) the character of rales is altered or rales can disappear for a short time after coughing, while pleural friction sound does not change in these conditions; (2) when a stethoscope is pressed tighter against the chest, the pleural friction sound is intensified, while rales do not change; (3) crepitation is only heard at the height of inspire tion, while pleural friction sound is heard during both inspiration and ex-
Chapter 5. Respiratory System
" ration; (4) if a patient moves his diaphragm in and out while his mouth Ld nose are closed, the sound produced by the friction of the pleura due to the movement of the diaphragm can be heard, while rales and crepitation cannot because there is no air movement in the bronchi.
Succusion (Hippocratic) sound. This is the splashing sound heard in the chest of a patient with hydropneumothorax, i.e. when serous fluid and air are accumulated in the pleural cavity. The sound was first described by Hippocrates, hence the name. The sound can be identified by auscultation: the physician presses his ear against the chest of the patient and then shakes the patient suddenly. The splashing sounds are sometimes heard by the patient himself during abrupt movements.
Bronchophony. This is the voice conduction by the larynx to the chest, as determined by auscultation. But as distinct from vocal fremitus, the words containing sounds 'r' or 'ch' are whispered during auscultation. In physiological conditions, voice conducted to the outer surface of the chest is hardly audible on either side of the chest in symmetrical points. Exaggerated bronchophony (like exaggerated vocal fremitus) suggests consolidation of the pulmonary tissue (which better conducts sound waves) and also cavities in the lungs which act as resonators to intensify the sounds. Bronchophony is more useful than vocal fremitus in revealing consolidation foci in the lungs of a patient with soft and high voice.
Instrumental and Laboratory Methods
X-RAY EXAMINATION
Roentgenological methods used to examine the respiratory organs include roentgenoscopy, roentgenography, tomography, bronchography, and fluorography of the chest.
The most popular method of examination is roentgenoscopy of the lungs by which translucency of the lung fields may be determined. It is used to determine consolidation foci (indurations, pneumosclerosis, newgrowths) and cavities in the pulmonary tissue, foreign bodies of the trachea and bronchi, the presence of fluid or air in the pleural cavity, and also coarse pleural adhesions.
Roentgenography (radiography) is used for diagnostic purposes and for film recording of pathological changes in the respiratory organs discovered by roentgenoscopy. Some changes (indistinct focal consolidations, bron-chovascular pattern, etc.) can be better examined on a roentgenogram radiograph) rather than during roentgenoscopy.
Tomography gives layer-by-layer X-ray pictures of the lung. It is used Or more accurate diagnosis of the tumours and also small indurations, cavities and caverns in the lungs.
Special Part
Chapter 5. Respiratory System
Bronchography is used to study bronchi. After preliminary anaesthesia the radiopaque substance (iodolipol) is administered into the lumen of the bronchi. Roentgenograms (radiographs) of the lungs are then taken which give a distinct pattern of the bronchial tree. This method is used to reveal bronchiectasis, abscesses, and caverns in the lungs and contraction of the lumen in the bronchi by a tumour.
Fluorography is a variant of the X-ray examination method by which the image is made on a roll film of a small size. This is a convenient means for screening the population.
ENDOSCOPY