
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Inquiry 2 страница
|
|
Pathological deceleration of respiration occurs in functional inhibition °f the respiratory centre and its decreased excitability. It can be due to in-Creased intracranial pressure in patients with cerebral tumour, meningitis,
Special Part
Chapter 5. Respiratory System
cerebral haemorrhage, or oedema of the brain, and also due to the toxic efJ feet on the respiratory centre when toxic substances are accumulated in the^ blood, e.g. in uraemia, hepatic or diabetic coma, and in certain acute infecJ tious diseases.
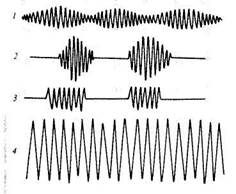
Respiration depth. The depth of breathing is determined by the volume of the inhaled and exhaled air at rest. This volume varies in an adult from 300 to 900 ml (500 ml on the average). Depending on depth, breathing can be either deep or superficial. Superficial (shallow) breathing often occurs in pathologically accelerated respiration when the length of the inspiration and the expiration phases becomes short. Deep breathing is, on the contrary, associated in most cases with pathological deceleration of the; respiration rate. Deep and slow respiration, with marked respiratory movements, is sometimes attended by noisy sounds. This is Kussmaul's respiration (Fig. 11) occurring in deep coma. In some pathological conditions, however, rare respiration can be shallow, while accelerated breathing deep. Rare superficial respiration can occur in sharp inhibition of the; respiratory centre, pronounced lung emphysema, and sharp narrowing of ] the vocal slit or the trachea. Respiration becomes accelerated and deep in high fever and marked anaemia.
Respiration rhythm. Respiration of a healthy person is rhythmic, of uniform depth and equal length of the inspiration and expiration phases. Rhythm of the respiratory centre can be inhibited in some types of oedema. Derangement of the respiratory function can cause oedema in which a series of respiratory movements alternates with a pronounced (readily detectable) elongation of the respiratory pause (lasting from a few seconds to a minute) or a temporary arrest of respiration (pnoea). This respiration is known as periodic.
|
Fig. 11. Spirograms in pathological respiration. a —Grocco's respiration; b — Cheyne-Stokes' respiration; 3 —Biot's respiration; 4 — Kussmaul's respiration.
Biot's respiration is characterized by rhythmic but deep respiratory ovements which alternate (at approximately regular intervals) with long piratory pauses (from few seconds to half a minute). Biot's respiration ccurs in meningitis patients and in agony with disorders of cerebral circulation.
Cheyne-Stokes' respiration is characterized by periods (from few
seconds to a minute) of cessation of respiration, followed by noiseless shallow respiration, which quickly deepens, becomes noisy to attain its maximum at the 5-7th inhalation, and then gradually slows down to end with a new short respiratory pause. During such pauses, the patient often loses his sense of orientation in the surroundings or even faints, to recover from the unconscious condition after respiratory movements are restored. This respiratory disorder occurs in diseases causing acute or chronic insufficiency of cerebral circulation and brain hypoxia, and also in heavy poisoning. More frequently this condition develops during sleep and is more characteristic of aged persons with marked atherosclerosis of the cerebral arteries.
Undulant (wave-like) Grocco's respiration somewhat resembles Cheyne-Stokes' respiration except that a weak shallow respiration occurs instead of the respiratory pause with subsequent deepening of the respiratory movement, followed by slowing down. This type of arrhythmic dyspnoea can probably be regarded as the early stages of the same pathological processes which are responsible for Cheyne-Stokes respiration.
PALPATION
Palpation is used as an additional means of examination to verify findings of observation (the shape of the chest, its dimensions, respiratory movements), for determining local or profuse tenderness of the chest, its elasticity (resilience), vocal fremitus, pleural friction and sounds of fluid in the pleural cavity.
Palpation should be done by placing the palms on the symmetrical (left and right) parts of the chest. This examination helps follow the respiratory excursions and deviation of the chest movements from their normal course. The epigastric angle is determined by palpation as well. The thumbs should be pressed tightly against the costal arch, their tips resting against the xiphoid process (ensiform cartilage).
Palpation is used to locate pain in the chest and its irradiation. For ex-
arnPle, in rib fracture, pain is localized over a limited site, namely at the
Point of the fracture. Displacement (careful!) of bone fractures will be at-
ended in this case by a specific sound (crunch). Inflammation of the inter-
Special Part
Chapter 5. Respiratory System
costal nerves and muscles also causes pain, but it can be felt during paiD tion over the entire intercostal space. Such pain is called superficial. It is; n~ tensified during deep breathing, when the patient bends to the affected side, or lies on this side.
Resilience or elasticity of the chest is determined by exerting pressure of the examining hands from the front to the sides of the chest or on the back and the sternum, and also by palpation of the intercostal spaces. The chest of a healthy person is elastic, plaint and yields under the pressure. In the presence of pleurisy with effusion, or pleural tumour, the intercostal space over the affected site becomes rigid. Rigidity of the chest increases in general in the aged due to ossification of the costal cartilages, development of the lung emphysema, and also with filling of both pleural cavities with fluid. Increased resistance of the chest can then be felt during examining the chest by compression in both the anteroposterior and lateral directions. Palpation is used for determining the strength of voice conduction to the chest surface (fremitus vocalis s. pectoralis). The palms of the hands are placed on the symmetrical parts of the chest and the patient is asked to utter loudly a few words (with the letter 'r' in them to intensify vibration). The voice should be as low as possible since voice vibrations are better transmitted by the air column in the trachea and the bronchi to the chest wall in this case. Fremitus vocalis can also be determined by one hand as well: the palm of the examining hand should be placed alternately on the symmetrical parts of the chest.
Vocal fremitus is of about the same intensity in the symmetrical parts of the chest of a healthy person. Vocal vibrations are louder in the upper parts of the chest and softer in its lower parts. Moreover, voice conduction is better in men with low voice and thin chest; the vibrations are weaker in women and children with higher voice (and also in persons with the well developed subcutaneous fat tissues). Vocal fremitus can be stronger or weaker (or in some cases it can even be impalpable) in pathological conditions of the respiratory organs. In focal affections, vocal fremitus becomes unequal over symmetrical parts of the chest.
Vocal fremitus is intensified when a part of the lung or its whole lobe becomes airless and more uniform (dense) because of a pathological process. According to the laws of physics, dense and uniform bodies conduct sound better than loose and non-uniform. Induration (consolidation) can be due to various causes, such as acute lobar pneumonia, pulmonary infarction, tuberculosis, accumulation of air or fluid in the pleural cavity, etc. Vocal fremitus is also intensified in the presence in the pulmonary tissue of an air cavity communicated with the bronchus.
Vocal fremitus becomes weaker (1) when liquid or gas are accumulated in the pleural cavity; they separate the lung from the chest wall to absorb
. e vibrations propagating from the vocal slit along the bronchial tree;
J2) in complete obstruction of the bronchial lumen by a tumour which in-
t rferes with normal conduction of sound waves to the chest wall; (3) in
sthenic emaciated patients (with weak voice); (4) in significant thickening
of the chest wall in obesity.
Low-frequency vibrations due to pleural friction (friction fremitus) in dry pleurisy, crepitation sounds characteristic of subcutaneous emphysema of the lungs, vibration of the chest in dry, low (low-pitch buzzing) rales can also be determined by palpation.
PERCUSSION
Depending on the object of examination, various methods of percussion are used to examine the lungs. The examination begins with comparative percussion.
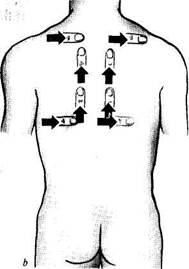
Comparative percussion. A certain sequence is followed in comparative percussion. Percussion sounds over the lung apices (in the front) on the symmetrical points of the chest are first compared; the pleximeter finger is placed parallel to the clavicle. The plexor finger is then used to strike the clavicle which is used as a pleximeter in this case. During percussion of the lungs below the clavicle, the pleximeter finger is placed in the interspace at the strictly symmetrical points of the left and right sides of the chest. The percussion sounds are compared only to the level of the 4th rib along the medioclavicular line (and medially). The heart lying below this level changes the percussion sound. For comparative percussion of the axillary region, the patient should raise his arms and clamp the hands at the back of the head. Comparative percussion of the lungs on the back begins with suprascapular areas. The pleximeter finger is placed horizontally, while during percussion of the regions between the scapulae, the pleximeter should be vertical. The patient should cross his arms on the chest to displace the scapulae anteriorly (away from the backbone). During percussion of the points lying below the scapulae, the pleximeter should again be horizontal; in the interspace it should be placed parallel to the ribs (Fig. 12a and b).
Percussion sounds of the lungs of a healthy person cannot be of equal strength, length or pitch even if the percussion blows are uniform at symmetrical points. This depends on the mass and thickness of the pulmonary ayer and also on the influence of the adjacent organs on the percussion sound. It is softer and shorter (1) over the right upper lobe because it is °cated somewhat below the left (due to the shorter right upper bronchus) and also because of the better development of the muscles of the apt side of he shoulder girdle; (2) in the second and third interspace on the left,
Special Part
Chapter 5. Respiratory System
|
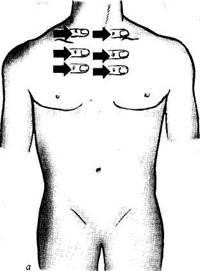
Fig. 12. Comparative percussion on the anterior (a) and posterior (b) surfaces of the chest.
because of the closer location of the heart; (3) over the upper lobes of the lung (compared with the lower lobes) because of the varying thickness of pneumatic pulmonary tissue; (4) in the right axillary region (compared with the left one) because of the closer location of the liver. The difference in percussion sounds here depends on the fact that the diaphragm and the lung border on the left with the stomach whose bottom is filled with air and gives a loud tympanic sound during percussion (Traube's semilunar space). The percussion sound in the left axillary region is therefore louder and higher (with tympanic character) because of the resonant effect ('air bladder') of the stomach.
The percussion sound can change in pathological processes because of the decreased content or full absence of air in a part of the lung, and because of the pleural fluid (transudate, effusion, blood), increased airiness of the lung tissue, and the presence of air in the pleural cavity (pneumothorax).
The amount of air in the lungs decreases in (1) pneumosclerosis, fibrous-focal tuberculosis, (2) pleural adhesion or obliteration of the pleural cavity which interferes with normal distention of the lung during inspiration; the difference in the percussion sound will be more pronounced at the inspiration level and weaker during the expiration; (3) lobular and especially confluent pneumonia, in which pulmonary tissue alternates with consolidations; (4) considerable oedema of the lungs, especially in the in-
feriolateral regions due to insufficient contractility of the left ventricle; (5) compression of the pulmonary tissue by the pleural fluid (compression atelectasis) above the fluid level; (6) complete obstruction of the large bronchus with a tumour and gradual resorption of air from the lungs below the closure of the lumen (obstructive atelectasis). Clear pulmonary sounds become shorter and higher (i.e. duller) in the mentioned pathological conditions. If these conditions are attended by decreased tension in the elastic elements of the pulmonary tissue, e.g. in the presence of compression or obstructive atelectasis, the sound over the atelectatic zone becomes dull with a tympanic tone. This sound can also be heard during percussion of a patient with acute lobar pneumonia at its first stage, when the alveoli of the affected lobe, in addition to air, contain also a small amount of fluid.
A complete absence of air in the entire lobe of the lung or its part (segment) is observed in the following cases: (a) acute lobar pneumonia at the consolidation stage, when the alveoli are filled with the inflammatory ex-udate containing fibrin; (b) formation in the lung of a large cavity, which is filled with the inflammatory fluid (sputum, pus, echinococcous acid, etc.), or heterogeneous airless tissue (tumour); (c) accumulation of fluid in the pleural cavity (transudate, exudate, blood). Percussion over airless parts of the lung or over fluid accumulated in the pleural cavity gives a soft short and high sound which is called dull or, by analogy with the percussion sounds of airless organs and tissues (liver, muscles), liver dullness. But the absolute dullness identical to the percussion sound of the liver can only be heard in the presence of a large amount of fluid in the pleural cavity.
The amount of air in the lung increases in emphysema. The percussion sound in lung emphysema is louder than the dull tympanic sound because of the increased airiness of the pulmonary tissue and decreased elasticity of the tense pulmonary tissues; but the tympanic character is preserved. The percussion sound resembles the one produced by a stroke on a box; hence the name bandbox sound.
The amount of air held inside the lung increases with formation in it of a smooth-wall cavity filled with air and communicated with the bronchus (abscess, tuberculotic cavern). The percussion sound over this area will be tympanic. If the cavity is small and situated deeply in the chest, vibrations °f the pulmonary tissue will not reach this cavity and no tympanic sound will be heard. Such a cavity will only be revealed by roentgenoscopy. The sound over a very large smooth-wall cavity in the lung (6—8 cm in diameter) will be tympanic, resembling a stroke on a metal (metallic percussion sound). If this cavity is located superficially and is communicated Wlth the bronchus through a narrow slit, the percussion sound will be soft and will resemble that of a cracked pot (hence the name—cracked-pot sound).
Special Part
Chapter 5. Respiratory System
Fig. 13. Determining the superior border of the lung on the anterior surface of the chest.
Fig. 14. Determining the position of the lung apex over the clavicle.
Fig. 15. Determining the inferior border of the lung in the right parasternal, midclavi-cular, and anterior axillary line.
Fig. 16. Determining the inferior border of the lung in the scapular line.
Topographic percussion. Topographic percussion is used for determining (1) the upper borders of the lungs or the upper level of their apices and their width (Kroenig's area); (2) the lower borders of the lungs, and (3) variation mobility of the lower border of the lung.
The position of the upper borders (apices) of the lungs is determined both anteriorly and posteriorly. In order to locate the apex of the lung, the pleximeter finger is placed parallel to the clavicle (Fig. 13) and percussion is effected from the middle upwards and slightly medially, to dullness. The upper level of the apices in healthy persons is 3—4 cm above the clavicles (Fig. 14). The upper posterior border of the lungs is always determined by their position with respect to the spinous process of the 7th cervical vertebra. The pleximeter finger is placed over the supraspinous fossa, parallel to the scapular spine and stroked from the middle. The pleximeter finger is moved gradually upward to the point located 3—4 cm laterally to the spinous process of the 7th cervical vertebra, at its level, and percussion is then continued until dullness. Normal height of the lung apices (posterior) is about at the level of the spinous process of the 7th cervical vertebra.
The so-called Kroenig's area is a band of clear resonance over the lung apices. The width of these areas is determined by the low anterior border of the trapezius muscle and is (on an average) 5—6 cm wide, but its width can vary from 3 to 8 cm. The anterior border of the trapezius muscle divides
the Kroenig area into its anterior field which extends to the clavicle, and the posterior one that widens toward the supraspinous fossa. Light or subliminal percussion is used to determine the width of the lung apex. The pleximeter finger is held over the middle portion of m. trapezius, perpendicular to its anterior margin, and percussion is first carried out medially, and then laterally, to dullness. The distance between the points of transition of the clear pulmonary resonance to dullness is measured in centimetres.
The upper border of the lungs and the width of the Kroenig area can vary depending on the amount of air in the apices. If the amount of air is high (which may be due to emphysema) the apices increase in size and move upwards. The Kroenig area widens accordingly. The presence of connective tissue in the lung apex (which usually develops during inflammation as in tuberculosis or pneumonia or inflammatory infiltration) decreases the airiness of the pulmonary tissue. The upper border of the lung thus lowers and the width of the Kroenig area decreases.
. To outline the lower borders of the lungs their percussion is carried out in the downward direction along conventional vertical topographical lines. fhe lower border of the right lung is first determined anteriorly along the Parasternal and the medioclavicular lines, then laterally along the anterior, medial and posterior axillary lines (Fig. 15), and posteriorly along the Papular and paraspinal lines (Fig. 16). The lower border of the left lung is
Special Part
r
Chapter 5. Respiratory System
determined only laterally, by the three axillary lines, and posteriorly by the scapular and paraspinal lines. The lower border of the left lung is not determined anteriorly because of the presence of the heart. The pleximeter finger is placed in the interspaces, parallel to the ribs, and the plexor finger produces slight and uniform strokes over it. Percussion of the chest is usually begun anteriorly, from the second and third costal interspace (with the patient in the lying or upright position). The examination of the lateral surface of the chest is performed from the axillary fossa (arm pit). The patient either sits or stands with the hands behind the back of the head. The examination ends with the posterior percussion from the seventh costal interspace, or from the scapular angle, which ends at the seventh rib.
The lower border of the right lung is as a rule at the point of transition of the clear pulmonary resonance to dullness (lung-liver border). In exceptional cases, when air is present in the abdominal cavity (e.g. in perforation of gastric or duodenal ulcer), liver dullness may disappear. The clear pulmonary resonance will then convert to tympany. The lower border of the left lung by the anterior and midaxillary lines is determined by the transition of clear pulmonary resonance to dull tympany. This is explained by the contact between the lower surface of the lung (through the diaphragm) and a small airless organ, such as the spleen and the fundus of the stomach, which give tympany (Traube's space).
Table 1
| Normal Lower Border of the Lungs | ||
| Percussion point | Right lung | Left lung |
| Parasternal line | 5th costal interspace | |
| Midclavicular line | 6th rib | ________ |
| Anterior axillary line | 7th rib | |
| Midaxillary line | 8th rib | 8th rib |
| Posterior axillary line | 9th rib | 9th rib |
| Scapular line | 10th rib | 10th rib |
| Paraspinal line | Spinous process of 1 lth thoracic vertebra | Spinous process of 11th thoracic vertebra |
The lower borders of the lungs in normosthenic persons usually occur as given in Table 1. The position of the border varies depending on the constitutional properties of the body. The lower border of the lungs in asthenic persons is slightly lower than in normosthenics and is found at the interspace (rather than on the rib as in normosthenics) whereas this border is
slightly higher in hypersthenic persons. The lower border of the lungs rises temporary during late pregnancy.
The position of the lower border of the lungs can vary in various pathological conditions that develop in the lungs, the pleura, the diaphragm, and the abdominal viscera. The border can both rise and lower from the normal level. This displacement can be uni- or bilateral.
Bilateral lowering of the lower border of the lungs can occur in acute and chronic dilation of the lungs (attack of bronchial asthma and emphysema of the lungs, respectively) and also in sudden weakening of the tone of the abdominal muscles and lowering of the abdominal viscera (splanchnoptosis). Unilateral lowering of the lower border of the lungs can be due to vicarious (compensatory) emphysema of one lung with inactiva-tion of the other lung (pleurisy with effusion, hydrothorax, pneumothorax, hemiparesis of the diaphragm).
The elevation of the lower border of the lungs is usually unilateral and occurs in (1) shrivelling of the lung due to development of connective tissue (pneumosclerosis); (2) complete obstruction of the lower-lobe bronchus by a tumour which causes gradual collapse of the lung, atelectasis; (3) accumulation of fluid or air in the pleural cavity which displace the lung upwards and medially toward the root; (4) marked enlargement of the liver (cancer, echinococcosis), or of the spleen (chronic myeloleukaemia). Bilateral elevation of the lower borders of the lungs occurs in the presence of large amounts of fluid (ascites) or air in the abdomen due to an acute perforation of gastric or duodenal ulcer, and also in acute meteorism.
After determining the lower border of the lungs at rest, respiratory mobility of pulmonary borders should be determined by percussion during forced inspiration and expiration. This mobility is called active, and is usually measured by the difference in the position of the lower border of the lungs between the two extremes. Measurements are done by three lines on the right side (midclavicular, axillary, and scapular lines) and two lines on the left side (midaxillary and scapular lines). The normal variation of the lower border of the lungs is described by the figures given in Table 2. Mobility of the lower border of the left lung by the midclavicular line cannot be determined because of the interference of the heart.
The respiratory mobility of the lungs is determined as follows. The lower border of the lungs in normal respiration is first determined and marked by a dermograph. The patient is then asked to make a forced inspiration and to keep breath at the height. The pleximeter finger should at this moment be held at the lower border of the lung (determined earlier). Percussion is now continued by moving the pleximeter downwards to complete dullness, where the second mark should be made by a dermograph at the upper edge of the pleximeter finger. The patient is then asked to exhale
Special Part
Chapter 5. Respiratory System
Table 2
Respiratory Mobility of the Lower Border of Normal Lungs
| Topographic line | Mobility of the lower border of the lung, in cm | |||||
| right lung | left lung | |||||
| inhalation | exhalation | total | inhalation | exhalation | total | |
| Midclavicular line Midaxillary line Scapular line | 2-3 3-4 2-3 | 2-3 3-4 2-3 | 4-6 6-8 4-6 | 3-4 2-3 | 3-4 2-3 | 6-8 4-6 |
| Fig. 17. Determining the mobility of the lower lung border in the midclavicular line. |
maximum air from the lungs and to keep breath again. The percussion is now continued in the upward direction until the clear vesicular resonance appears. The third dermographic mark should be made at the point where relative dullness is heard. The distance between the extreme marks is measured (Fig. 17). It corresponds to the maximum respiratory mobility. The patient in a grave condition is unable to keep breath and another method is recommended to determine the respiratory mobility of the lungs.

After marking the lower border of the lung in quiet breathing, the patient is asked to make deep inhalations and exhalations without keeping breath. Percussion should be continuous during deep breathing and the nleximeter finger should gradually move downwards. First the percussion sound is loud and low during inhalation and soft and high during exhalation. Soon a point is attained where the sounds become of the same pitch and strength during both inhalation and exhalation. This point is the lower border of the lung at forced inspiration. The lower border at forced exhalation is determined in the same way.
Respiratory mobility of the lower border of the lungs is diminished in inflammatory infiltration or congestive plethora of the lungs, decreased elasticity of the pulmonary tissue (emphysema), profuse pleural effusion, and in pleural adhesion or obliteration.
The so-called passive respiratory mobility is determined in some diseases. This is the mobility of the lung borders during changes in the posture. When the patient changes his posture from the upright to horizontal one, the lower border of the lungs descends some 2 cm, while the lower border of the right lung of a patient lying on his left side may lower 3-4 cm. In pathological conditions, e.g. in pleural adhesion, the variation of the lower border of the lungs is markedly limited.
AUSCULTATION
Like percussion, auscultation of the lungs should be carried out according to a plan. Stethoscope or phonendoscope should be placed in strictly symmetrical points of the right and left sides of the chest (Fig. 18). Auscultation begins with the anterior wall of the chest, from its upper part, in the supra- and subclavicular regions, and then the stethoscope should be moved downward and laterally. The lungs are then auscultated in the same order from the posterior wall of the chest and in the axillary regions. In order to increase the area of auscultation between the scapulae, the patient should be asked to cross his arms on the chest and in this way to displace his shoulder-blades laterally from the spine, while for convenience of auscultation of the axillary regions he should place his hands on the back of the head.
The posture does not matter, but the patient should better sit up on a stool with his hands on the laps. The patient may stand, but the physician should remember that deep breathing (hyperventilation of the lungs) may cause vertigo and the patient may faint. Bearing this in mind, and also to ensure a tight contact between the stethoscope and the skin (especially if a °ie-piece stethoscope is used) the physician should always use his free hand 0 support the patient on the side opposite to the point of application of the stethoscope bell.