
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Special Pathology. Among the very great number of various diseases of the respiratory organs, most common are inflammatory affections of the bronchi (acute and chronic
|
|
Among the very great number of various diseases of the respiratory organs, most common are inflammatory affections of the bronchi (acute and chronic bronchitis, bronchiectasis), of pulmonary tissue (acute and chronic pneumonia, less frequently destructive affections such as abscess or gangrene of the lungs), and of the pleura (pleurisy, empyema). The lungs are affected selectively only in tuberculosis. The incidence of tuberculosis was high in old times. Certain occupational hazards (silicons and the like) can cause special forms of inflammatory diseases of the lungs provided safety measures are not taken and the exposure becomes chronic. Diseases with a protracted course, and also inadequately treated inflammatory diseases (or in decreased reactivity of the body) can terminate in focal or diffuse pneumosclerosis. Frequent are tumours of the lungs (bron-chogenic cancer, metastases into the lungs of cancer tumours of other organs). Pulmonary vessels are also often affected (embolism, lung infarction); these affections may also include affections due to foreign bodies of the bronchi, injuries to the lung (contusion, compression, etc.), congenital abnormalities (cysts, etc.), and genetically determined systemic diseases with lung affections (mucoviscidosis, deficit of alpha-1-antitrypsin, etc.); comparatively often occur allergic diseases (bronchial asthma), and many other pulmonary pathologies.
Bronchitis
Bronchitis is inflammation of the bronchi. The disease stands first in the list of respiratory pathologies and occurs mostly in children and the
aged.
Primary and secondary bronchitis are distinguished. In primary bronchitis, inflammation develops as the primary process in the bronchi. Secondary bronchitis attends other diseases, such as influenza, whooping cough, measles, tuberculosis, chronic diseases of the lungs and the heart. According to the type of the inflammatory reaction bronchitis is subdivided into catarrhal, mucopurulent, purulent, fibrinous, and haemorrhagic. Bronchitis can also be focal or diffuse, depending on the localization of inflammation. Inflammatory process can reside only in the trachea and large bronchi (tracheobronchitis), the bronchi of the fine and medium calibre (bronchitis), or in the bronchioles (bronchiolitis, occurring mostly in infants). According to the course of the disease, acute and chronic bronchitis are differentiated.
ACUTE BRONCHITIS
Aetiology and pathogenesis. Acute bronchitis can arise (1) in acute infectious diseases, such as influenza, whooping cough, measles, and the like; (2) in chills which decrease the body's resistance to microbes (saprophytes) that are present in the upper air ways, i.e. pneumococci, pneumobacilli (Klebsiellae), streptococci, etc. Mechanical and chemical factors, such as coal, cement or lime dusts, formaldehyde, acids, or acetone may promote the onset of the disease. Asthenia (especially after grave diseases) and chronic sinusitis and rhinitis are also predisposing factors to the development of acute bronchitis.
Pathological anatomy. The disease begins with hyperaemia and swelling of the bronchial mucosa, hypersecretion of mucus and diapedesis of leucocytes; then follows desquamation of epithelium and formation of erosions; in grave bronchitis, inflammation may involve the sub-mucous and muscular layers of the bronchial walls and peribronchial interstitial tissues.
Clinical picture. The patient feels discomfort in the throat and retrosternal smarting. The voice becomes hoarse, the patient feels weakness, and excess perspiration develops. Cough is first dry or with expectoration of scant tenacious sputum; cough may be coarse, resonant, sometimes barking; it may come in excruciating attacks. Sputum is expectorated on the second or the third day of the disease. First it is nuicopurulent, sometimes with streaks of scarlet blood; then it becomes Purulent; coughing gradually subsides and softens.
The body temperature in focal bronchitis is normal or subfebrile; in grave diffuse bronchitis it may rise to 38-39 °C. The respiration rate in-
Special Part
Chapter 5. Respiratory System
creases insignificantly; it can only accelerate to 30—40 per minute in diffuse affections of fine bronchi and bronchioles. Dyspnoea and tachycardia develop.
Percussion sounds over the lungs are usually unchanged. Auscultation reveals harsh breathing and dry buzzing and whistling rales, which often change their character and amount after cough. During resolution of inflammation in the bronchi, tenacious sputum is thinned by the action of proteolytic enzymes contained in it, and moist dulled rales may be heard together with dry rales. X-ray examination in acute bronchitis does not reveal any changes. The leucocyte count of the blood may rise to 9000—11000 in one microlitre. ESR slightly increases. The sputum is mucous or mucopurulent, sometimes with streaks of blood; it contains columnar epithelium and other cell elements. Fibrin clots (bronchial casts) are expectorated in acute fibrous bronchitis.
Course. The patient usually recovers in two or three weeks. Under the effect of some aggravating factors, such as smoking or chilling, or in the absence of timely treatment, the disease may run a protracted course or become complicated with bronchopneumonia.
Treatment. Antibiotics and sulphonamides, broncholytics (ephedrine or isoprenaline) in combination with expectorants, e.g. thermopsis infusion (1: 200), a tablespoonful three times a day, alkaline inhalations and other remedies are prescribed. Antibiotics and broncholytics should better be taken as aerosols. Also recommended are cups, mustard plasters and compresses on the chest, foot baths.
Prophylaxis. Hardening of the body (cool showers, bathing); removal of irritants of the upper air ways (smoking, occupational hazards) and treatment and prevention of chronic diseases of the nose and throat.
CHRONIC BRONCHITIS
Chronic bronchitis is chronic inflammation of the bronchi and bronchioles.
Aetiology and pathogenesis. Infection is an important factor in development and further course of the disease. Chronic bronchitis may develop after acute bronchitis or pneumonia. Chronic occupational inhalation of dusts or chemicals, and also residence in cities with moist climate and frequent fluctuations of the weather conditions, are also predisposing factors. No less important factor for the development of chronic bronchitis is smoking: bronchitis occurs in 50—80 per cent of habitual smokers while its incidence among non-smoking population is only 7—19 per cent. Autoimmune allergic reactions occurring due to absorption of products of protein decomposition (that are formed in the lungs in inflammatory foci) are important factors for persistent chronic bronchitis.
Pathological anatomy. At the early stage of the disease, the mucosa is plethoric, cyanotic, and hypertrophic at some points. Mucous glands are hyperplastic. Inflammation eventually involves the submucous and muscle layers, where cicatricial tissue develops. The mucosa and cartilaginous lamina become atrophied. Bronchial walls become thin to increase the lumen and to cause bronchiectasis. The peribronchial tissue can also be involved in the process with subsequent development of interstitial pneumonia. Interalveolar septa become gradually atrophied and lung emphysema develops; the number of capillaries of the pulmonary artery decreases. Muscular hypertrophy of the right ventricle and also right-ventricular incompetence may join the pulmonary insufficiency.
Clinical picture. The picture of chronic bronchitis depends on the degree of bronchial involvement and on the depth of affection of the bronchial wall. The main symptoms of chronic bronchitis are cough and dyspnoea. Cough may differ in character and change depending on the season and weather. In dry weather, especially in summer, cough is mild and dry, or it may be absent. At increased air humidity and in rain, cough intensifies, while in the cold season it becomes persistent and intense, with expectoration of tenacious mucopurulent or purulent sputum. Sputum is sometimes so thick that it is expectorated in the form of fibrinous bands that look like casts of the bronchial lumen (fibrinous bronchitis).
Dyspnoea in chronic bronchitis is not only due to the lung hypoventila-tion but also due to lung emphysema that develops as a secondary process. The character of dyspnoea is mostly mixed. First difficult breathing occurs only during exercise such as ascending a hill or upstairs. Further dyspnoea becomes more pronounced. In diffuse inflammation of fine bronchi, dyspnoea becomes expiratory. The disease may be attended by the general symptoms such as weakness, rapid fatigue, excess perspiration; temperature rises in exacerbation of bronchitis.
Inspection, palpation and percussion of the chest, and also X-ray examination do not reveal any changes in non-complicated chronic bronchitis. In grave chronic bronchitis, when pneumosclerosis, pulmonary emphysema, and cardiopulmonary insufficiency attend the main process, accessory muscles become actively involved in the respiratory act, the neck veins become swollen, and cyanosis develops. In this case percussion of the lungs gives a bandbox sound; mobility of the lower border of the lung is limited. Breathing can be vesicular, harsh, or (when emphysema develops) weakened vesicular. Buzzing and whistling dry (less frequently moist) rales are also heard on auscultation.
The blood picture only changes in exacerbation of bronchitis. The changes include increased leucocyte counts and accelerated ESR.
Sputum of a patient with chronic bronchitis is mucopurulent or purulent. In putrefactive bronchitis, sputum is greenish-brown or brown because of decomposed blood; the smell is offensive. Microscopy reveals a great number of leucocytes, degrading erythrocytes, and ample coccal flora.
Special Part
Chapter 5. Respiratory System
X-ray examinations in chronic bronchitis, complicated by developing pneumosclerosis or lung emphysema, reveal signs of these diseases. Deformation of the bronchi may be revealed on bronchography. Bronchoscopy gives a picture of atrophic (less frequently hypertrophic) bronchitis (with thinning or swelling of the bronchial mucosa).
Course. The course of chronic bronchitis varies. It may persist for many years, but the signs of the anatomical and functional changes are mildly pronounced. In other patients chronic bronchitis progresses slowly to give exacerbations on chills and during epidemic outbreaks of influenza, or under the effect of some occupational hazards. Recurrent bronchitis and peribronchitis give bronchiectases and often pneumonia. Obstruction of bronchial patency provokes the development of emphysema and car-diopulmonary insufficiency.
Treatment. In chronic bronchitis treatment is aimed at eradication and subsequent prevention of exacerbations (the patient should be kept under regular medical observation). The inflammatory process in the bronchi should be removed. In aggravation of chronic bronchitis sulpha drugs (sulphadimethoxin, 1-1.5 g a day and ethasol syn. sulphaethidole) and antibiotics are prescribed. If the disease is protracted and aggravated by asthma, broncholytics are given in addition. Corticosteroids, which have anti-allergic and anti-inflammatory action, are given in some cases. To lessen cough, antitussives (codeine and libexin) and expectorants (thermop-sis infusion, 1.0: 200.0, a tablespoonful 3—4 times a day) are prescribed. Harmful occupational and domestic factors (smoking in particular) should be removed.
Climate therapy favours recovery. Warm marine climate is especially helpful.
Prophylaxis consists in removal of harmful factors provoking the onset of inflammation of the bronchi (e.g. smoking), improvement of working conditions (especially in industry where air may be contaminated with dusts, etc.), treatment of chronic diseases of the upper airways, and strengthening the organism's defence forces (hardening by cool showers, swimming, exercises, walks, etc.).
Bronchial Asthma
Bronchial asthma is an allergic disease which is manifested by paroxysmal attacks (Gk asthma panting).
Aetiology and pathogenesis. Bronchial asthma is a polyaetiological disease. It can be provoked by external agents (exogenic allergens) and internal causes (endogenic allergens that usually depend on the infections of the airways). Non-infectious allergic (atopic) and infectious-allergic asthma are distinguished accordingly.
Attacks of asthma can be provoked by various odours, such as those of flowers, hay, perfumes, petrol, carpet or pillow dusts, moulds (in damp rooms), the smell of ursol dyes, asbestos dust; by some foods such as eggs, crabs, strawberries (food asthma), and medicinal preparations. An attack of asthma can sometimes be provoked not by the allergen itself but by memory of it or by remembrance of the conditions under which the allergen acted in the past. The patient can develop an asthmatic attack when he reappears in a certain room or a house or street, where he once had an attack, or even by remembrance of this particular room, house, street,
etc.
Endogenic allergens causing attacks of asthma include microbial antigens that are formed during various inflammatory processes,.such as sinusitis, chronic bronchitis, chronic pneumonia, etc. Products of decomposition of microbes and tissue proteins forming due to proteolytic process at the inflammatory focus can act as allergens.
Asthma is an allergic disease in which the body is sensitized mainly by the substances of protein nature; other substances and effects can also provoke the disease.
The allergen becomes active in the body only under certain conditions. Bronchial asthma and its attacks develop when the body's reactivity is changed. An important factor promoting sensitization of the body and pathological reactivity is the hereditary-constitutional factor. Climate is also important in this respect. For example, attacks of asthma more often occur during spring or autumn; they can be removed in certain climatic zones, e.g. in highland conditions, or, on the contrary, they may be intensified. Attacks are more likely to occur in cold and damp weather. Pathological response of the parasympathetic nervous system to stimuli received from various exteroceptors and interoceptors, hyperexcitation of the vagus nerve centres, development of pathological reactions in the afferent receptors of the bronchial walls and their hypersensitivity to local irritants are also important factors in the development of asthma attacks. There is evidence of the importance of partial /3-adrenergic blockade in the pathogenesis of bronchial asthma and reduced activity of cyclic adenosine monophosphate (intracellular mediator) during attacks of the disease. Finally, certain hormonal shifts are also important, which in the first instance is connected with the adrenal glands. This is confirmed, in particular, by the favourable effect of corticosteroid therapy on the course of the disease.
It has recently been established that attacks of asthma are provoked by an allergic reaction occurring in the bronchial tissue. Three stages in the course of an attack of atopic bronchial asthma, which proceeds as an allergic reaction of the immediate type, are distinguished. In the first (im-munological) stage the antigen combines with the specific antibodies
Special Part
Chapter 5. Respiratory System
III
reagins (the IgE class compounds fixed mainly on mast, plasma, and lymph cells); in the second (pathochemical) stage histamine, serotonin, a slow-acting substance anaphylactin, and other biologically active substances are released from these cells as a result of degranulation and alteration; in the third (pathophysiological) stage, spasms develop in the bronchi along with the exudative reaction and oedema of the bronchial mucosa, as the result of the action of the above mentioned substances. An attack of an infectious-allergic asthma develops in the same way, but a delayed (cellular) allergic reaction may be involved in its origination.
Pathological anatomy. Macroscopic study of the lungs of patients who died from an attack of asthma reveals diffuse or irregular focal emphysema. Bronchi contain thick tenacious secretion that clogs the lumen of separate small bronchi and causes atelectasis. The bronchial mucosa is markedly hyperaemic and swollen. Microscopy shows desquamation of the epithelium, thickening of the basal membrane, hypertrophy of the muscular layer and eosinophilic infiltration of the bronchial wall.
Clinical picture. The classical description of bronchial asthma was given in 1838 by G. I. Sokolsky. An attack of allergic asthma begins abruptly and acutely and usually quickly subsides. Attacks of dyspnoea developing against the background of chronic infectious diseases of the respiratory ducts (infectious-allergic asthma) are often not severe but protracted. Signs of chronic bronchitis, pneumosclerosis, and lung emphysema can be revealed in such patients in periods clear of paroxysms.
Attacks of dyspnoea in bronchial asthma are quite similar; they arise suddenly, gradually increase in strength, and last from a few minutes to several hours and even several days. A prolonged attack of asthma is called status asthmaticus. During such an attack, the patient has to assume a forced attitude; he usually sits in bed, leans against his laps, his breath is loud, often whistling and noisy, the mouth is open, the nostrils flare out. The veins of the neck become swollen during expiration and return to norm during inspiration. At the peak of an attack, the patient begins coughing with poorly expectorated thick and tenacious sputum. The chest expands during an attack (to the size of the chest during inspiration). Accessory respiratory muscles are actively involved in the respiratory act. Percussion of the lungs gives the bandbox sound, the lower margins of the lungs are below normal, the mobility of the lower borders is sharply limited during both inspiration and expiration. Auscultation reveals many whistling rales against the background of weakened vesicular respiration with a markedly prolonged expiration. The whistling rales are sometimes heard even at a distance. Tachycardia is usually observed. The borders of complete dullness of the heart cannot be determined because of the acute inflation of the lungs. By the moment the attack abates the sputum thins and expec-
toration becomes easier: high and dry rales in the lungs determined by auscultation decrease to give ways to low buzzing and often moist non-consonant rales of various calibres; the attack of dyspnoea gradually abates.
Blood test during attacks shows moderate lymphocytosis and eosinophilia. The sputum contains 40 to 60 per cent of eosinophils and often Curschmann spirals and Charcot-Leyden crystals.
X-ray examination of the thoracic organs during an attack of asthma shows high translucency of the lung fields and limited mobility of the diaphragm.
Patients with uncomplicated bronchial asthma have no complaints in the periods clear of attacks. Physical, X-ray, and laboratory examinations reveal no changes except eosinophilia of the blood.
Course. Attacks of asthma sometimes occur very rarely (once a year or even several years). Some patients develop a more severe course with frequent and grave attacks. Concurrent chronic bronchitis, pneumosclerosis, and emphysema of the lungs cause the corresponding changes detectable by routine examinations; cardiopulmonary insufficiency gradually develops. In rare cases the patient may die during an attack.
Treatment. The provoking factor should be first identified and eliminated whenever possible. The removal of the causative stimulus will prevent the development of the disease. The allergen can be identified by sensitivity skin tests using suspected substances in special allergological laboratories. Once the allergen is known, desensitization should be attempted. Foci of infection should be treated in infectious-allergic asthma (bronchitis, bronchiectasis, sinusitis, etc.). Unfortunately it is not always easy to remove the cause of bronchial asthma or to carry out effective pathogenic therapy. Symptomatic therapy should then be given to remove or prevent attacks of asthma.
An attack of asthma can be removed by subcutaneous injections of 0.2-1 ml of a 0.1 per cent adrenaline hydrochloride solution or 1 ml of a 5 Per cent ephedrine solution. Euphylline (aminophylline) is given intravenously. Broncholytics are also prescribed (inhalations included). A Protracted status asthmaticus is an indication to corticosteroid therapy. To Prevent attacks of bronchial asthma, broncholytics are given in courses. Remedial exercises and health-resort therapy are also indicated.
Acute Pneumonia
Pneumonia is an acute inflammation of the lungs developing either independently or as a complication in other diseases. Pneumonia is promi-neiit among other diseases of the internal organs. It prevails in epidemic in-

|
Special Part
Chapter 5. Respiratory System
fluenza. Men are more susceptible to the disease than women; it is especially severe in children and elderly patients.
An aetiological classification of pneumonia has been adopted. Differentiated are bacterial pneumonia (pneumococcal, staphylococcal, strep-tococcal, etc.), virus (caused by the influenza virus, viruses or ornithosis, psittacosis), mycotic (candidiasis, etc.) and pneumonia caused by irritating gases, vapours, dusts, etc. It has long been established that the clinical aspects of bacterial pneumonia somewhat vary depending on the initial body's reactivity. This mainly refers to pneumonia caused by pneumococ-cus, especially of types I and II. Sometimes the disease is hyperergic, which accounts for its special acuity, cyclic character of its course, frequent affection of the whole lobe of the lung (with involvement of the pleura) and a special character of effusion due to a markedly impaired permeability of the vessel wall (the presence of fibrin and erythrocytes in the effusion). As distinct from more frequently occurring bronchopneumonia (syn.: focal, catarrhal, lobular pneumonia), this pneumonia is called croupous (syn.: acute lobar, fibrinous pneumonia, pleuropneumonia). Pleuropneumonia was formerly diagnosed very frequently but now it rarely occurs in its typical form.
BRONCHOPNEUMONIA (FOCAL PNEUMONIA)
Separate lobules of the lungs are affected in bronchopneumonia, hence another name, lobular pneumonia. Inflammatory foci may be multiple, or they may fuse (confluent pneumonia); the foci may be located in various parts of both lungs simultaneously (mostly in the lower parts of the lungs).
Aetiology and pathogenesis. Quite varied bacterial flora would be normally found in bronchopneumonia. The wide use of antibiotics has changed the proportion of microbes that are found in pneumonia. The importance of pneumococci has significantly decreased while the role of other microorganisms, especially of streptococci and staphylococci, has increased. Acute pneumonia is caused in many cases by viruses (in influenza, ornithosis, and psittacosis).
In addition to the infectious factor, predisposing conditions are also very important. They decrease the immunological properties of the body (overcooling, acute respiratory diseases, etc.). Bronchopneumonia can develop against the background of chronic diseases of the lungs (bron-chiectasis, chronic bronchitis) due to haematogenic infection in purulent inflammatory diseases (sepsis, after operations, etc.). Aged patients with long-standing and severe diseases or subjects with plethoric congestion of the lungs can develop hypostatic pneumonia. Aspiration of foreign bodies (food, vomitus, etc.) causes aspiration pneumonia. Inhalation of suf-
focating or irritating gases or vapours (benzene, toluene, benzine, etc.) or other toxic substances can also provoke the onset to bronchopneumonia. The aetiological factor is often decisive for the clinic and course of pneumonia, but irrespective of aetiology, there are always some general signs of the disease.
Development of bronchopneumonia is associated with the extension of the inflammatory process from the bronchi and bronchioles to the pulmonary tissue (hence another name of bronchopneumonia—catarrhal pneumonia, which reflects the transition of inflammation and infection with the mucous secretion from the inflamed bronchi into the alveoli). Infection gets inside the pulmonary tissue via the bronchi, and more frequently peribronchially, i.e. by lymph ducts and interalveolar septa. Local atelectasis that occurs in obstruction of the bronchus by a " mucopurulent plug" (N. Filatov) is important in the pathogenesis of bronchopneumonia. Obstruction of bronchial patency can be caused by a sudden bronchospasm and oedema of the bronchial mucosa, inflammation (bronchitis), etc. Recently bronchopneumonia occurs mostly in children and the aged, usually during cold seasons (spring, autumn, winter).
Pathological anatomy. The microscopic picture of inflammatory foci in bronchopneumonia is quite varied because of the different persistence of the foci. The alveoli at the site of inflammation are filled with serous or mucous effusion containing large amounts of leucocytes. If bronchopneumonia is associated with influenza, microscopy shows the rupture of fine vessels. In confluent pneumonia, the inflammatory foci fuse together to involve several segments or even the whole lobe of the lung.
Clinical picture. The onset of the disease is usually overlooked because it often develops against the background of bronchitis or catarrh of the upper airways. The findings of physical examination of the patient at the onset of bronchopneumonia are the same as in acute bronchitis. Sites of consolidated tissue are often small and difficult to reveal by X-ray examination. But if a patient with clinical signs of acute bronchitis develops high temperature and has symptoms of a more severe disease, he should be considered to have bronchopneumonia (M. Konchalovsky).
The most typical signs of bronchopneumonia are cough, fever, and dyspnoea. If the inflammatory focus is at the periphery of the lung and the inflammation involves the pleura, pain in the chest during coughing and deep breathing may occur. Fever may persist for various terms in bronchopneumonia. Usually fever is remittent and irregular. The temperature is often subfebrile or it may even be normal in the middle-aged or old patients..
Objective examination can sometimes reveal moderate hyperaemia of the face and cyanosis of the lips. Respiration accelerates to 25—30 per min;
Special Part
Chapter 5. Respiratory System
respiratory lagging of the affected side of the chest may be observed. Percussion and auscultation may prove ineffective if the inflammatory foci are small and deeply located. In the presence of a large focus, especially if it is located at the periphery of the lung tissue, and also in confluent pneumonia, the percussion sounds lose resonance (or become completely dull), and auscultation reveals vesiculobronchial or bronchial breathing. Vocal fremitus and bronchophony are characteristic of such cases. Dry and moist rales are frequent, but consonating moist rales and crepitation that are heard over a limited part of the chest are especially informative. X-ray examination reveals indistinct densities; in confluent pneumonia densities are spotted (mostly in the lower portions of the lungs). The shadows of the lung roots may be expanded due to enlarged lymph nodes. X-ray examination of the lungs reveals focal inflammations at least 1—2 cm in diameter; very small and separated foci of consolidated lung tissue are undeterminable; therefore in the absence of the X-ray signs of pneumonia the diagnosis of bronchopneumonia cannot be rejected in the presence of clinical symptoms.
Sputum is mucopurulent, first tenacious but later more thin, sometimes there are traces of blood, but it is not rusty. It contains a great number of leucocytes, macrophages and columnar epithelium. Bacterial flora is varied and ample. But it is scant in virus pneumonia. The blood count shows mild neutrophilic leucocytosis, a certain shift to the left, and a moderately increased ESR.
Course. Bronchopneumonia is usually more protracted and flaccid than pleuropneumonia. Prognosis is favourable with appropriate treatment. But the disease can transform into its chronic form. Bronchopneumonia can be aggravated by abscess of the lung and bronchiec-tasis.
ACUTE LOBAR PNEUMONIA
Aetiology and pathogenesis. All authors who studied the aetiology of acute lobar pneumonia (pleuropneumonia, crupous pneumonia), discovered Frenkel pneumococci (mostly types I and II, less frequently types III and IV) in about 95 per cent of cases. Fridlaender diplobacillus, Pfeiffer's bacillus, streptococcus, staphylococcus, etc. are found less frequently.
Acute lobar pneumonia occurs mostly after severe overcooling. The main portal of infection is bronchogenic, less frequently lymphogenic and haematogenic. Congestion in the lungs in cardiac failure, chronic and acute diseases of the upper airways, avitaminosis, overstrain and other factors promote the onset of pneumonia. Acute lobar pneumonia is relatively fre-
quent in patients who had pneumonia in their past history (it recurs in 30-40 per cent of cases which is another evidence of the hyperergic character of the disease).
Pathological anatomy. Four stages are distinguished in the course of acute lobar pneumonia. The stage of congestion is characterized by acute hyperaemia of the lung tissue, exudation, obstruction of capillary patency, and stasis of the blood. It lasts from 12 hours to 3 days. The stage of red hepatization continues from 1 to 3 days. The alveoli are filled with plasma rich in fibrinogen and erythrocytes: The stage of grey hepatization is characterized by cessation of erythrocyte diapedesis; the erythrocytes contained in the exudate decompose and their haemoglobin converts into haemosiderin. The alveoli (containing fibrin) become filled with leucocytes. The lungs become grey. The stage lasts from 2 to 6 days. The last stage is resolution. Fibrin is liquefied by proteolytic enzymes and exudate is gradually resorbed.
Clinical picture. The onset of the disease. Typical acute lobar pneumonia begins abruptly with shaking chills, severe headache, and fever (to 39-40 °C). The chills usually persist for 1-3 hours, then pain appears in the affected side; sometimes it may arise below the costal arch in the abdomen to simulate acute appendicitis, hepatic colics, etc. (this usually occurs in inflammation of the lower lobe of the lung, when the diaphragmal pleura becomes involved in the process). Cough is first dry and in 1—2 days rusty sputum is expectorated. The patient's general condition is grave.
General examination shows hyperaemia of the cheeks, more pronounced on the affected side, dyspnoea, cyanosis, often herpes on the lips and nose; the affected side of the chest lags behind in the respiratory act. Vocal fremitus is slightly exaggerated over the affected lobe. Sounds over the lungs are quite varied and depend on the distribution of the process, the stage of the disease, and other factors. At the onset of the disease, shortened percussion sound can be heard over the affected lobe, often with tympanic effect because liquid and air are simultaneously contained in the alveoli; the vesicular breathing is decreased while bronchophony is increased; the so-called initial crepitation (crepitus indux) is present.
The height of the disease (classified by pathologists as the red and grey hepatization stages.) is characterized by the grave general condition. It can be explained not only by the size of the affected area of the lung which thus does not take part in respiration but also by general toxicosis. Respiration is accelerated and superficial (30-40 per min) and tachycardia (100-200 beats per min) is characteristic. Dullness is heard over the affected lobe of the lung; bronchial respiration is revealed by auscultation; vocal fremitus and bronchophony are exaggerated. Vocal fremitus is in some cases either absent or enfeebled (in combination with pleurisy with effusion, and also lri massive acute lobar pneumonia, in which the inflammatory exudate fills large bronchi); bronchial breathing is inaudible. Before the antibiotic era, tne patient with acute lobar pneumonia would often develop vascular
Special Part
Chapter 5. Respiratory System
failure with a marked drop in the arterial pressure due to toxicosis. Vascular collapse is attended by general asthenia, drop of temperature, increased dyspnoea, cyanosis, and accelerated and small pulse. The nervous system is also affected (sleep is deranged, hallucinations and delirium are possible, especially in alcoholic patients). The heart, liver, kidneys and some other organs are also affected. Fever persists for 9-11 days if antibiotics or sulpha drugs are not given. The temperature then drops either abruptly during 12-24 hours or lytically, during more than 2-3 days.
Resolution stage. The exudate thins, air again fills the alveoli to decrease dullness of the percussion sound, tympany increases, and bronchial breathing lessens. Crepitation is heai -1 again (crepitus redux) because the alveolar walls separate as air fills them. Moist rales are heard. Exaggerated vocal fremitus, then bronchophony, and finally bronchial breathing disappear. The leucocyte count in the blood increases to 15 x x 109-25 x 109 per litre (15 000-25000 per microlitre); neutrophils account for 80—90 per cent of the leucocytes; a shift to the left with the appearance of juvenile forms is sometimes observed. The number of eosinophils decreases and they can disappear completely in grave cases. Relative lymphopenia and monocytosis are observed. The ESR increases. The red blood does not change.
Sputum is tenacious during the congestion period; it is slightly crimson and contains much protein, a small number of leucocytes, erythrocytes, alveolar cells, and macrophages. In the stage of red hepatization sputum is scant and rusty; it contains fibrin and a higher number of formed elements. In the stage of grey hepatization leucocyte count in the sputum increases significantly; the sputum becomes mucopurulent. In the resolution stage, leucocytes are converted into detritus, which is found in the sputum; many macrophages are also found. Pneumococci, staphylococci, Friedlaender diplobacilli can be detected in the sputum.
X-Ray changes in the lungs depend on the stage of the disease. The lung pattern is first intensified, then dense foci develop, which later fuse. The shadow usually corresponds to the lung lobe (Fig. 24). The lungs become normally clear in two or three weeks. Dynamics of the X-ray changes depends on the time when the therapy is begun.
Course and complications. Fatal outcomes in acute lobar pneumonia were formerly 20—25 per cent. Before antibiotics and sulpha drugs came into wide use, complications (purulent processes in the lungs and pleurisy, usually purulent) were frequent; their incidence has now decreased significantly. If pleurisy develops before resolution of pneumonia, it is called parapneumonic. If it occurs after resolution, it is referred to as metapneumonic pleurisy. Other complications occur as well:
Fig. 24. X-ray of the upper lobe of the left lung in acute lobar pneumonia.
myocarditis, meningitis, and focal nephritis. If resolution of the exudate is delayed, and connective tissue grows into it, cirrhosis of the affected lobe of the lung develops (carnification). Mortality from acute lobar pneumonia has recently decreased significantly.
Treatment of pneumonia. The patient should be hospitalized and kept in bed. Food should be rich in vitamins and easily assimilable. Antibiotics (penicillin, 300000-500000 units, 4 to 6 times a day intramuscularly, streptomycin, tetracycline, and other antibiotics) and sulpha drugs (sulphadimezine, sulphaethidole, sulphadimethoxine, etc.) are the main preparations for treating pneumonia. Oxygen therapy (an oxygen mask or a tent) is also helpful. It improves metabolism and has a favourable effect on the cardiovascular system. Vascular insufficiency is treated by coffein and camphor; in the presence of heart failure, digitalis and strophanthine Preparations are given. Expectorants (thermopsis, etc.) should be given, especially during the resolution of pneumonia; cups, mustard plaster, and Physiotherapy accelerate elimination of residual effects of pneumonia. Respiratory exercises are important to improve lung ventilation.
Prophylaxis mainly consists in strengthening and hardening of the body.
178 Special Part
Pulmonary Abscess
Pulmonary abscess is a purulent melting of the lung tissue circumscribed by an inflammatory swelling.
Aetiology and pathogenesis. The aetiological factor in the development of a purulent process in the lungs is mostly the coccal flora (streptococci, staphylococci, and pneumococci). The disease is sometimes associated with saprophytic autoinfection of the upper airways. The development and intensity of the purulent process in the lungs depend on the reactivity of the lung tissue and of the entire body.
The purulent process in the lungs develops mostly as an outcome of pneumonia or complicated bronchiectasis. Primary abscesses of the lungs arise in wounds to the chest, aspiration of foreign bodies, and after operations on the upper airways (tonsillectomy and the like). Pulmonary abscess can develop also by a haematogenic or lymphogenic routes, when the infection is carried into the lungs from a purulent focus in the body. The lung tissue can be resorbed without the involvement of microbes. In lung infarction, or in the presence of a degrading tumour, a cavity may be formed due to local disorder in blood circulation. In such cases necrotization of the lung tissue can be the precursor of a purulent process. Suppuration of an echinococcal cyst in the lung can be another cause.
Pathological anatomy. Pulmonary abscesses are characterized by the presence of a single or multiple purulent foci that may be found in one or both lungs. After the abscess opens, a cavity is formed which is surrounded by inflammatory infiltration. Acute abscesses are surrounded by a thin ridge of the inflamed tissue. Chronic abscesses are encapsulated in fibrous tissue.
Clinical picture. Two periods are distinguished: before and after opening of an abscess. The first period is formation of the abscess. It continues for 10—12 days, on the average. At the onset of the disease patients complain of general indisposition, weakness, chills, cough with meagre sputum, and pain in the chest. Fever is first moderate but gradually becomes remittent, and then hectic. Dyspnoea develops even in the presence of a small abscess.
Palpation of the chest can in some cases detect painfulness in the intercostal spaces of the affected side. This symptom is associated with involvement in the process of the costal pleura. Unilateral thoracic lagging corresponding to inflammation may be observed. Vocal fremitus depends on the location of the inflammatory focus. It is often exaggerated in peripheral location and remains unchanged in deep location of the inflammatory focus.
Percussion can determine loss of resonance (or dull sound) on the affected side. Auscultation in small deep abscesses does not reveal any abnor-
Chapter 5. Respiratory System
malities. If the abscess is superficial, respiration over the affected side is decreased and vesicular, sometimes with a bronchial character. In some cases breathing is harsh, and dry rales can be heard.
The blood picture is an important and objective criterion in the diagnosis of lung abscess. Neutrophilic leucocytosis, 15 x 109-25 x 109 per litre (15 000-20000 per microlitre), is observed; a shift to the left, to the myelocytes, is also characteristic. The ESR increases significantly. Study of the sputum is not specific before the abscess opens.
The X-ray picture of the abscess during the first period of the disease does not differ from that in common pneumonia or tuberculous infiltration: a large focus of increased density with rough and indistinct margins is determined.
The clinical picture of the second period begins with the opening of the purulent abscess into the bronchus. There may be a transitory condition between the first and second periods of the disease during which the main clinical symptoms are intensified (elevated temperature with great circa-dian variations, heavy cough, dyspnoea, pain in the chest, etc.). Rupture of the abscess into the bronchus is attended by a sudden release of ample purulent sputum (" full mouth"), sometimes with offensive odour, which on standing separates into two or three layers: mucous, serous, and purulent. Further expectorations will depend on the volume of the cavity and vary from 200 ml to 1-2 1 a day. Objectively the patient looks feverish. If the pleura is involved, unilateral thoracic lagging is observed on the affected side. After the cavity is free from pus, and depending on its location and size, physical findings may be different. Tympany is determined in the presence of large and superficial abscesses by percussion. Respiration can be either bronchovesicular or bronchial; if a large cavity containing air communicates with the bronchial lumen, respiration can be amphorical. Resonant moist moderate and large bubbling rales are usually heard over a limited area. In the presence of concurrent diffuse bronchitis, intense rales interfere with location of the abscess.
Neutrophilic leucocytosis with a shift to the left and increased ESR are observed. In grave and protracted cases, iron-deficiency (hypoferric) anaemia develops.
On standing, sputum separates into three layers: the upper (foamy and mucous), the middle (liquid, serous) and the bottom layer (pus). Microscopy of the sputum reveals the presence of elastic fibres (in addition to many leucocytes and erythrocytes). The absence of elastic fibres in the sputum indicates termination of degradation of the lung tissue. Bacteriological flora is ample, mostly containing cocci; in the presence of antibiotic therapy the flora is meagre.
X-raying of the emptied abscess shows a specifically increased
Special Part
Chapter 5. Respiratory System
Fig. 25. X-ray of abscess in the right lung.
translucency. Variation of the liquid level (Fig. 25) can be observed with variation of the patient's posture. If the draining bronchus is at the bottom of the cavity (which is common with abscesses of the lung apices), the liquid level is undeterminable (the fluid flows down and is withdrawn through the outlet bronchus). The abscess cavity is surrounded on all sides by a border of inflamed tissue with a diffuse outer contour.
Course. Development of the lung abscess and its healing depend on location of the cavity, conditions for its emptying, and concurrent complications. In most cases abscesses heal with formation of focal pulmonary fibrosis at the site of the common cavity, but in 30-40 per cent of patients recovery is incomplete and the disease becomes chronic. Chronic diseases of the lungs (bronchiectasis, pulmonary fibrosis, etc.) promote a protracted course of pulmonary suppuration. The following complications of the lung abscess are distinguished: (1) rupture of the abscess into the pleural cavity with development of pyopneumothorax; (2) pulmonary haemorrhage; (3) development of new pulmonary abscesses; (4) metastases of the abscesses into the brain, liver and other organs. Complications aggravate the prognosis of the disease.
Treatment. Bed-rest regimen in hospital is necessary. Antibiotics and sulpha drugs should be given as early as possible. Penicillin and strep-
tomycin should be given along with broad-spectrum antibiotics such as tetracycline (0.2-0.3 g 4-6 times a day after meals, oletetrin, etc.). Sulpha drugs (sulphadimidine, sulphadimethoxine, etc.) should be given in sufficiently large doses and for a long period. In addition to peroral or intramuscular administration, antibiotics should be given intratracheally or as aerosols (1-2 times a day for 2-4 weeks). Therapeutic bronchoscopy is widely used to remove pus from the cavity and to administer antibiotics directly into it. Symptomatic treatment consists in prescribing expectorants and broncholytics (ephedrine, drotaverine, and others) which liquefy sputum. Adequate draining is very important for a better emptying of the cavity: the patient should find a posture at which sputum withdrawal is the best and to assume this posture for 30 minutes two or three times a day. If conservative therapy proves ineffective, surgical treatment should be given in a month or two (earlier, in grave cases). The operation consists in removal of the lobe (or the whole lung if abscesses are multiple).
Pleurisy
Pleurisy is inflammation of the pleura. Dry pleurisy (pleuritis sicca) and pleurisy with effusion (pleuritis exudativa) are distinguished. The character of the inflammatory effusion may be different: serous, serofibrinous, purulent, and haemorrhagic.
Aetiology and pathogenesis. Serous and serofibrinous pleurisy attend tuberculosis (in 70-90 per cent of cases), and pneumonia, certain infections, and also rheumatism in 10—30 per cent of cases. The purulent process in the pleura may be caused by pneumococci, streptococci, staphylococci, and other microbes. Haemorrhagic pleurisy arises in tuberculosis of the pleura, bronchogenic cancer of the lung with involvement of the pleura, and also in injuries to the chest.
Most diseases of the pleura (pleurisy included) are secondary to disease of the lung. Pleurisy usually develops as a reaction of the pleura to pathological changes in the adjacent organs, in the lungs in the first instance, and less frequently as a symptom of a systemic disease (polyserosites of various aetiology). Serous pleurisy often arises as an allergic reaction. Purulent pleurisy is often a complication of bron-chopneumonia: inflammation may extend onto the pleura, or an inflammatory focus may turn into an abscess which opens into the pleural cavity. Inflammation of the pleura is always attended by markedly increased Permeability of the wall of the affected capillaries of the pulmonary pleura.
Reactivity of the body is a very important factor in the pathogenesis of Pleurisy. In fibrinous or dry pleurisy fibrin precipitates from the exudate (which is produced in a small amount) and gradually deposits on the
ic n,
Special Part
Chapter 5. Respiratory System

|
|
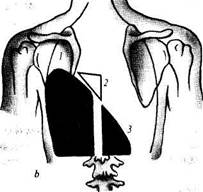
| Fig. 26. Percussion and auscultation in pleurisy with effusion. |
pleura. Serous pleurisy may become infected to convert into purulent; ex-udate becomes turbid and contains many leucocytes. In the presence of purulent processes in the lungs or adjacent organs (pericarditis, perioesophagitis, etc.), purulent pleurisy often develops abruptly. The affection of the pleura in tumours, which in most cases are metastatic (less frequently primary), decreases its absorptive function to promote accumulation of pleural effusion (haemorrhagic effusion in most cases).
Pathological anatomy. Dry pleurisy is characterized by thickening of the pleura and deposition of fibrin in it. Pleural membranes become dull and hyperaemic; commissures and sometimes more significant adhesions develop. Pleurisy with effusion is characterized by the presence of exudate in the pleural cavity, mostly in the outer costal-diaphragmatic sinus. Parietal, supradiaphragmatic and interlobar pleurisy also occur. After abatement of inflammation, effusion (serous, serofibrinous, haemorrhagic, purulent) usually resolves but the pleura remains thickened, its membranes adhere to one another, and the pleural cavity is completely obliterated in some cases. Effusion sometimes remains between adhesions to stimulate encapsulated pleurisy.
DRY PLEURISY
Clinical picture. A characteristic symptom of dry pleurisy is pain in the chest which becomes stronger during breathing and coughing. Cough is usually dry, the patient complains of general indisposition; the temperature is subfebrile. Respiration is superficial (deep breathing intensifies friction of the pleural membranes to cause pain). Lying on the affected side lessens the pain. Inspection of the patient can reveal unilateral thoracic lagging during respiration. Percussion fails to detect any changes except decreased mobility of the lung border on the affected side. Auscultation determines pleural friction sound over the inflamed site. X-ray picture shows limited mobility of the diaphragm because the patient spares the affected side of his chest.
The blood picture remains unchanged but moderate leucocytosis is observed in some cases.
Course. Dry pleurisy has a favourable course and the patient recovers completely in one or three weeks.
PLEURISY WITH EFFUSION
Clinical picture. Patients suffering from pleurisy with effusion usually complain of fever, pain or the feeling of heaviness in the side, and dyspnoea (which develops due to respiratory insufficiency caused by compression of the lung). Cough is usually mild (or absent in some cases). The patient's general condition is grave, especially in purulent pleurisy, which is attended by high temperature with pronounced circadian fluctuations,
chills, and signs of general toxicosis. Inspection of the patient reveals asymmetry of the chest due to enlargement of the side where the effusion is accumulated; the affected side of the chest usually lags behind in respiratory movements. Vocal fremitus is not transmitted at the area of fluid accumulation.
Percussion over the area of fluid accumulation produces dullness (Fig. 26). The upper limit of dullness is usually the S-shaped curve (Damoiseau's curve) whose upper point is in the posterior axillary line. The effusion thus occupies the area, which is a triangle both anteriorly and posteriorly. The Damoiseau curve (Fig. 27) is formed because exudate in pleurisy with effusion more freely accumulates in the lateral portions of the

Fig. 27. Pleurisy with effusion.
a—anterior vtetf; fo—posterior view; /—Damoiseau's curve; 2—Garland's triangle; 3— Rauchfuss-Grocco
triangle.
Special Part
Chapter 5. Respiratory System
|
| it. _ |
pleural cavity, mostly in the costal-diaphragmatic sinus. As distinct from effusion, which is restricted by adhesions, transudate more freely presses the lung and the Damoiseau curve is not therefore determined. In addition to the Damoiseau curve, two triangles can be determined by percussion in pleurisy with effusion. The Garland triangle is found on the affected side and is characterized by a dulled tympanic sound. It corresponds to the lung pressed by the effusion, and is located between the spine and the Damoiseau curve. The Rauchfuss-Grocco triangle is found on the healthy side and is a kind of extension of dullness determined on the affected side. The sides of the triangle are formed by the diaphragm and the spine, while the continued Damoiseau curve is the hypotenuse. The triangle is mainly due to displacement of the mediastinum to the healthy side. Mobility of the lower border of the lung on the affected side is not usually determined in pleurisy with effusion. Left-sided pleurisy with effusion is characterized by the absence of the Traube space (the left pleural sinus is filled with effusion and a dulled percussion sound is heard over the gastric air bubble instead of the tympany).
Respiration in the region of accumulated effusion is not auscultated, or it can be very weak. Respiration auscultated slightly above the effusion level is usually bronchial which is due to compression of the lung and displacement of air from it. Vocal fremitus and bronchophony over the effusion are not determined because the vibrating walls of the bronchi that conduct voice are separated from the chest wall by the fluid. The heart is usually displaced by the effusion toward the healthy side. Tachycardia is observed. Arterial pressure may be decreased. Dizziness, faints, etc., sometimes occur because of the marked toxicosis.
A radiograph of the thoracic organs (Fig. 28) shows a homogeneous density whose area corresponds to the area of dullness. If effusion is scarce, it accumulates in the outer sinus. Large volumes of effusion cover the entire lung to its apex and displace the mediastinum toward the intact side to lower the diaphragm. The encapsulated parietal pleurisy gives the picture of parietal density. The medial border is usually sharply outlined. Density of the interlobar pleurisy extends along the interlobar sulcus in the form of a triangle or a spindle. Diaphragmatic pleurisy is characterized either by a limited mobility of the diaphragm or its complete absence. The upper border of the effusion is convex (upward) to follow the curvature of the diaphragm.
Exploratory puncture is necessary in order to determine the properties of the exudate for accurate diagnosis. The fluid obtained by pleural puncture is studied at the laboratory.
During the initial stage of the disease the blood picture may show mild leucocytosis (marked leucocytosis is characteristic of purulent pleurisy) and
Fig. 28. X-ray of the left lung in pleurisy with effusion.
sometimes eosinophilia. The ESR is increased. Tuberculosis pleurisy is characterized by lymphocytosis, while rheumatic pleurisy by neutrophilosis.
Course. The course of pleurisy with effusion depends on the aetiology of the affection. Pleurisy in rheumatism would normally resolve in 2-3 weeks (with appropriate treatment). Pleurisy with effusion complicating pneumonia (metapneumonic pleurisy, usually serous) also has a comparatively mild course. A protracted course is characteristic of pleurisy with effusion of tuberculous aetiology. Development of coarse adhesions interferes with resorption of the effusion (encapsulated pleurisy), while a prolonged purulent process may result in amyloidosis of the internal organs.
Resorption of effusion may be followed by some specific residual phenomena, such as sunken chest and the absence of diaphragmatic mobility on the affected side, displacement of the mediastinal organs toward the affected side, and sometimes permanent pleural friction.
Treatment. This, in the first instance, includes the therapy of the main disease, such as rheumatism (salicylates, amidopyrine, corticosteroids), pneumonia (sulpha drugs, and antibiotics), tuberculosis (PASA, phthivazide, streptomycin, canamycin, and others). Symptomatic therapy
Special Part
Chapter 5. Respiratory System
includes general strengthening (vitamins, etc.), desensitizing preparations, and high-calorie diet. Thermal procedures (compresses, diathermy) are useful to accelerate the resolution process. If pleural fluid is not resorbed during 2—3 weeks, evacuation of the effusion is necessary. Purulent ex-udate should obligatory be removed. Withdrawal of the fluid should be slow to avoid collapse or faint. As a rule, 0.5-1 1 of effusion is removed and antibiotics are injected instead into the pleural cavity. In order to accelerate resorption of the effusion, diuretics can be given. In the presence of cardiac failure, cordiamine, strophanthine and similar preparations are indicated. To prevent pleural adhesion during resorption of the exudate, remedial exercises should be prescribed.
Prophylaxis. Prevention of serofibrinous pleurisy consists in early diagnosis and active treatment of tuberculosis, rheumatism and other diseases which may provoke pleurisy, and also in strengthening of the body (exercises, cool shower, etc.).
Chronic Pneumonia
Aetiology and pathogenesis. Chronic pneumonia often develops as a result of protracted bronchopneumonia. Its development is facilitated by frequent recurrent inflammations in the bronchi and the lungs, influenza epidemics, inhalation of harmful chemicals, smoking, etc. Involvement of auto-immune processes helps conversion of acute and subacute diseases of the lungs into the chronic form. In most cases no specific causative agents are found in chronic pneumonia; streptococci, staphylococci, and pneumococci would be usually revealed by inoculation tests. If pneumonia is cured incompletely, the inflammatory process becomes slow (interstitial pneumonia) to give finally focal or diffuse pneumosclerosis. Bronchiectasis is formed in such patients, or they may develop emphysema and respiratory insufficiency.
Pathological anatomy. Areas of chronic inflammation in the lungs are observed along with the growth of connective tissue (focal or diffuse). Inflammatory changes may involve the bronchial walls and pleura; pulmonary vessels become stenosed and even obliterated.
Clinical picture. Many patients with chronic pneumonia (especially the aged) may have normal temperature, the amount of expectorated sputum may be small, and there may be no changes in the blood. Dyspnoea, subfebrile temperature, permanent cough with expectoration of purulent or mucopurulent sputum, mild leucocytosis are found in some patients. Percussion may fail to reveal loss of resonance over the affected side due to a concurrent emphysema. Auscultation of the affected side reveals fine and moderate moist rales, sometimes againts the background of dry diffuse
rales. X-ray examination is important: the interlobar septa are thickened, the lung pattern in the region of the inflammation is intensified, and the lung root is changed (enlarged lymph nodes).
The course of the disease is usually protracted and slowly progressing. Three stages of the disease are distinguished in this country. The first stage of chronic pneumonia is protracted pneumonia (lasting over 6 weeks) and chronic bronchitis concurrent with relapsing pneumonia. The second stage is characterized by frequent exacerbations of the inflammation in the lungs alternating with more or less prolonged remissions in the presence of symptoms of pneumosclerosis, lung emphysema and bronchiectasis. The third stage is characterized by marked symptoms, frequent exacerbations and pronounced functional disorders of external respiration and circulation.
Treatment. Combined treatment is necessary. Broad-spectrum antibiotics should be used with their frequent alternation to prevent microbial resistance to a particular antibiotic. For example, oletetrin is given per os for 5-10 days (250 mg 4-6 times a day), then it is replaced by the sodium salt of ampicillin (250—500 mg 4—6 times a day intramuscularly). Combination of antibiotics with sulpha drugs is effective. Bronchial draining is necessary in addition to the antibiotic therapy. It can be stimulated by giving expectorants, such as thermopsis preparations or ammonium chloride. In certain cases, corticosteroids are prescribed together with antibiotics to suppress auto-immune processes.
Bronchiectasis
This is a condition characterized by dilatation of the bronchi. Bron-chiectatic conditions are divided into primary (congenital, which are very rare) and secondary (secondary to various diseases of the bronchi, lungs and pleura).
As an independent (and frequently occurring) disease bronchiectasis has a specific clinical picture. It develops as a result of infection of bron-chiectases and in the presence of chronic inflammation in them. Bronchiectasis may also be regarded as a form of chronic non-specific pneumonia. The disease occurs at any age, but more commonly between the ages of 20 and 40. The incidence among men is 6—7 times higher than it is in women.
Aetiology and pathogenesis. Inflammation of bronchi and development of bronchiectasis in children can be the result of repeated acute bronchitis, whooping cough, measles, diphtheria, and sometimes tuberculous bronchoadenitis. Bronchiectases in youths and adults are formed due to acute diffuse bronchitis that develops against the background of chronic relapsing bronchitis, non-resolved pneumonia, and also lung abscess, in recurrent pneumonia, and pulmonary tuberculosis. Bronchiectases develop
Special Part
Chapter 5. Respiratory System
in bronchitis only when the inflammatory process extends onto the muscular layer of the bronchial wall or onto all its layers. Muscle fibres are destroyed, the bronchus tone is lost at this area and its walls become thin. The absence of ciliated epithelium at the inflamed portions of the bronchus promotes accumulation of sputum in its lumen, upsets its draining function, and thus stimulates chronic inflammation. The inflamed site is first granulated but later connective tissue develops which disfigures the bronchus. Severely affected portions of the bronchi dilate during intense coughing.
Pathological anatomy. Cylindrical, saccular, and fusiform bronchiectases are differentiated. They are mostly located in the lower lobes of the lungs. Severely affected bronchial walls are markedly destroyed. Inflammatory infiltration, granulation, and mature cicatricial tissues are found in these portions of the bronchi. Capillaries, arterioles, and smaller arteries of the bronchi are affected and blood flow in them is disturbed. Nerve endings and branches of the vagus that innervate the bronchus are also affected. Inflammation spreads onto the interstitial peribronchial tissue