
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Methods of Examination 3 страница. The mitral valve opening sound follows soon after the second heart
|
|
The mitral valve opening sound follows soon after the second heart
Fig. 33. Heart sounds in mitral stenosis. a— ECG; b— PCG; c—changes in the heart sounds: OS—sound of the mitral valve opening
sound to give it the character of reduplication. This sound is best heard at the heart apex rather than at the heart base; it is characterized by stability and is combined with other auscultative signs of mitral stenosis. The mitral valve opening sound is heard together with a loud (snapping) first sound characteristic of mitral stenosis, and the second sound, to form a specific triple rhythm (Fig. 33).
An extra-pericardial-sound can occur in pericardial adhesion. It originates during diastole, 0.08—0.14 s after the second sound, and is generated by the vibrating pericardium during the rapid dilatation of the ventricles at the beginning of diastole. The extra sound in adhesions in the pericardium can also arise during systole, between the first and the second heart sounds. This short and loud sound is also known as the systolic click.
Changes in heart sounds in heart diseases can be due to intensified physiological third or fourth sound. In normal subjects these sounds are better revealed in graphic recording (phonocardiography). But if the ventricular myocardium is much weakened, these sounds can be revealed by auscultation. Intensification of one of these sounds gives a three-sound rhythm, known as the gallop rhythm (because it resembles the galloping of a horse). The sounds of the gallop rhythm are usually soft and low, always
Special Part
Chapter 6. Blood Circulatory System
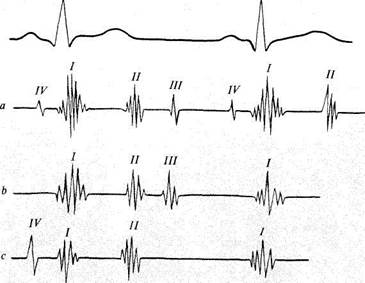
Fig. 34. Gallop rhythm.
a —four normal heart sounds; b —protodiastolic gallop rhythm formed due to intensification of the physiological third sound; c—presystolic gallop rhythm formed at the expense of the fourth sound.
attended by a thrust, for which reason they are best heard on direct auscultation; the gallop rhythm can also be heard in auscultation with a phonendoscope, but the patient should lie on the left side after a mild exercise. Protodiastolic (at the beginning of diastole), mesodiastolic (in the middle of diastole), and presystolic (at the end of diastole) gallop rhythms are distinguished by the time of appearance of the extra sound in diastole. Gallop rhythm is also classified as ventricular or atrial, according to its origin.
Protodiastolic gallop rhythm arises in considerably diminished tone of the ventricular myocardium. The ventricles distend quickly during their filling with blood at the beginning of diastole and the vibrations thus generated are audible as an extra sound. The sound appears 0.12-0.2 s after the second heart sound and is an increased physiological third sound (Fig. 34).
Presystolic gallop rhythm arises in intensification of the physiological fourth sound, which is due to the diminished tone of the ventricular myocardium and a stronger atrial contraction. Intensified contraction of
the overfilled atrium increases blood ejection into the ventricle, while a diminished tone of the ventricular myocardium causes quicker distention of its walls. The presystolic gallop rhythm is better detected in delayed atrioventricular conduction, when atrial systole is separated from the ventricular systole by a longer than normal period.
Both the third and the fourth heart sounds can intensify significantly in grave myocardial affection, but in tachycardia they sum up to give a mesodiastolic or summation gallop rhythm. Gallop rhythm is an important sign of myocardial weakness, and it has a great diagnostic and prognostic value. It develops in severe heart affections in patients with myocardial infarction, essential hypertension, myocarditis, chronic nephritis, decompen-sated heart diseases.
A pronounced acceleration of the cardiac rhythm makes the diastolic pause shorter so that it becomes almost as short as the systolic one. If the heart sounds heard at the cardiac apex are similar in intensity, a peculiar auscultative picture resembles the tic-tac or foetal rhythm, known also as embryocardial or pendulum rhythm. It occurs in severe cardiac failure, attacks of paroxysmal tachycardia, high fever, etc.
Cardiac murmurs. In addition to the normal heart sounds, abnormal sounds known as murmurs may be heard. Cardiac murmurs may be both endo- and exocardiac. Endocardiac murmurs occur most frequently. These may occur in anatomical changes in the structure of the heart valves (organic murmurs) or in dysfunction of the intact valves (functional murmurs). Functional murmurs may be heard with increased rate of blood flow or decreased blood viscosity. The mechanism of endocardiac murmurs can be easier understood if one remembers the laws of physics concerning the flow of liquids in tubes. If a tube has a point where its otherwise even lumen is narrowed, the passing liquid produces noise. This noise is associated with turbulent flow of liquid above the narrowed portion of the tube, which causes vibration of the tube. The intensity of noise depends on two factors, viz., the liquid velocity and the extent of narrowing. The higher the velocity of the liquid, the more intense is the noise; when the liquid velocity decreases, the noise lessens or disappears. As to the extent of tube narrowing, its influence on noise intensity is directly proportional only within a certain range. If the lumen is narrowed to a very high degree, noise may weaken or even disappear. Liquid is also set in vortex movement when it passes a narrow portion of the tube and enters its wider part again. The same reasons account for the murmurs that arise in the heart. If the passage is narrowed or on the contrary widened, blood is set in turbulent flow which generates murmurs. If the vascular lumen remains unchanged, murmurs may be produced by the changes in the blood flow rate, as is the case with thyrotoxicosis, fever, or nervous excitation. Decreased blood
Special Part
viscosity (e.g. in anaemia) increases the flow rate of blood and can also be the cause of murmurs. The most frequent cause of endocardiac murmur are various heart defects.
According to the time of appearance, murmurs are classified as systolic and diastolic. Systolic murmur occurs in cases when, during systole, blood moves from one chamber of the heart to another, or from the heart to the main vessels and meets an obstacle. Systolic murmur is heard in stenotic orifice of the aorta or the pulmonary trunk because blood ejected from the ventricles meets a narrowed vessel. Systolic murmur is also heard in cases with mitral and tricuspid incompetence. Generation of systolic murmur is explained by regurgitation of blood which is not completely expelled into the aorta and pulmonary trunk during the ventricular systole, but is partly returned to the atrium through an incompletely closed mitral or tricuspid orifice. Since this partly closed orifice is actually a narrow slit, murmur is generated as blood passes through it.
Diastolic murmur occurs if blood meets a narrowed passage during diastole. This murmur is heard in stenosed left or right atrioventricular orifice, since blood meets a narrow passage in its flow from the atria into the ventricles. Diastolic murmur also occurs in aortic or pulmonary valve incompetence. Murmur is generated when blood flows back from the vessels into the ventricles through a slit formed by incomplete closure of the cusps of the affected valve.
The following should be determined during auscultation: (1) the relation of the murmur to the phase of the heart activity (to systole or diastole); (2) the features, character, strength, and length of murmur; (3) localization of the murmur, i.e. the area where this murmur is heard best; (4) direction of transmission (radiation).
The relation of murmurs to systole or diastole is determined by the same signs that are used to differentiate between the first and the second heart sounds. Systolic murmur appears with the first heart sound, during a short pause of the heart; it is synchronous with the apex beat and the carotid pulse. Diastolic murmur follows the second sound, during the long pause of the heart. Three types of diastolic murmurs are distinguished: (1) protodiastolic murmur which arises at the very beginning of diastole, immediately after the second heart sound; (2) mesodiastolic murmur which is heard soon after the second heart sound; and (3) presystolic murmur which appears at the end of diastole (Fig. 35).
Properties of murmurs. By their character, murmurs may be soft, blowing, or on the contrary rough, grating or grazing sounds; musical murmurs can also be heard. By duration, heart murmurs are classified as short and long, and by their intensity as soft and loud. The intensity of the noise may change with the phase of the heart activity. Murmur may become
Chapter 6. Blood Circulatory System
systole diastole
|
| 1st sound 2nd sound |
| 1st sound |
Fig. 35. Relations between the heart sounds and murmurs.
A, B —systolic murmur: a —decrescendo; b —crescendo-decrescendo (diamond-shaped); Q D —diastolic murmur: c —presystolic; d —protodiastolic.
weaker (decrescendo) or louder (crescendo). Decrescendo murmurs occur more frequently. This can be explained as follows: as blood begins flowing from one heart chamber to another, or from the heart to the main vessel, the difference in pressures in two chambers is high and the blood flow rate is therefore high as well. But as the blood is expelled, the pressure inside the chamber from which the blood is ejected gradually decreases, the blood flow rate slows down, and the noise intensity decreases. Presystolic murmur has an increasing character and occurs mostly in stenosis of the anterior left atrioventricular orifice, at the very end of ventricular diastole,
Special Part
Chapter 6. Blood Circulatory System
when atrial systole begins to increase the blood outflow from the left atrium to the left ventricle.
The location of murmur corresponds to the best listening post of that particular valve where this murmur is generated. In certain cases, however, murmurs are better heard at a distance from the point where they are generated, provided their transmission is good. Murmurs are well transmitted in the direction of the blood flow. They are better heard in areas where the heart is close to the chest wall and where it is not covered by the lungs. Systolic murmur due to mitral valve incompetence is best heard at the heart apex. It can be transmitted by the firm muscle of the left ventricle to the axillary area or by the course of the backward blood flow from the left ventricle to the left atrium, i.e. into the second and third interspace, to the left of the sternum.
Diastolic murmur generated in a narrowed left atrioventricular orifice is usually heard over a limited area at the heart apex.
Systolic murmur due to stenosed aortic orifice is heard in the second interspace, to the right of the sternum. As a rule, it is well transmitted by the course of the blood flow onto the carotid arteries. Since this heart defect is characterized by a rough and loud (grating, grazing) sound, it can be determined in auscultation over the entire heart region and be transmitted to the interscapular space.
Diastolic murmur due to aortic valve incompetence is better heard not over the aortic valve but rather at the Botkin-Erb point, where it is transmitted by the back flow of blood from the aorta to the left ventricle.
Systolic murmur associated with tricuspid insufficiency is best heard at the base of the xiphoid process, since the right ventricle is the closest to the chest wall at this point, from which the sound can be transmitted upwards and to the right, in the direction of the right atrium. In the rare heart disease associated with stenosis of the right atrioventricular orifice, the diastolic murmur is heard over a limited area at the base of the xiphoid process.
It should be remembered that murmurs are best heard in certain postures of the patient. Systolic murmurs associated with incompetence of atrioventricular valves or with stenosis of the aortic or pulmonic orifice, are best heard with the patient in the recumbent posture because the blood flow from the ventricles is facilitated and the blood-flow rate increases. Diastolic murmurs arising due to stenosis of the atrioventricular orifice or incompetence of the aortic valve and the valve of pulmonary trunk are better heard in the upright position, since the blood flow to the ventricles from the atria or from the vessels (in insufficiency of the corresponding valves) is thus facilitated and the blood-flow rate increases.
Differentiation of murmurs. If several murmurs are heard
simultaneously over different valves, it is necessary to determine the affected valves and the character of their affections. Systolic and diastolic murmurs over one valve indicate its composite affection, i.e. incompetence of the valve and stenosis of the orifice. If systolic murmur is heard over one valve and diastolic murmur over the other, a combined affection of two valves can be diagnosed.
It is more difficult to decide whether one or two valves are affected if murmurs can be heard at various listening points during one and the same phase of heart activity. The character of the murmur should then be analysed. If a soft and blowing murmur is heard over one valve, and rough and grating over the other, the murmurs are generated by two different affected valves. By moving the stethoscope bell along the line connecting the two valves, the changes in the murmur intensity should be followed. If at some point of the line the murmur disappears or weakens markedly, and then again becomes louder, it will in most cases indicate affection of two valves. If the murmur decreases or increases as the stethoscope bell moves in the direction of the second valve, it usually indicates affection of only one valve. But this is not an indisputable sign because the degree of valve affection may differ too, and an independent, though less loud, murmur will then be heard over milder stenotic affection. The character of murmur transmission helps differentiation. For example, systolic murmur occurring in mitral valve incompetence is transmitted into the axillary region. It may be heard also over the aortic valve but it will not be transmitted onto the carotid arteries (as distinct from systolic murmur associated with stenosis of the aortic orifice).
During auscultation of the heart, it is necessary to differentiate between functional and organic, and between endocardial and exocardial murmurs. The following properties of functional murmurs help differentiate them from organic murmurs: (1) in most cases functional murmurs are systolic; (2) functional murmurs are not permanent and may arise and disappear when the person changes his posture, after exercise and during various respiratory phases; (3) they are mostly heard over the pulmonary trunk and less frequently over the heart apex; (4) functional murmurs are transient and are rarely heard during the entire systole; these are soft and blowing sounds; (5) the murmurs are normally heard over a limited area and are not transmitted to long distances from their source; (6) functional murmurs are not accompanied by other signs of valve affections (e.g. enlargement of the heart chambers or changes in the heart sounds).
Exocardial murmurs. Although synchronous with the heart work, they arise outside the heart. These are pericardial and pleuropericardial friction sounds.
Pericardial friction murmurs are connected with the changes in the
Special Part
Chapter 6. Blood Circulatory System
visceral and parietal pericardial layers in which fibrin is deposited (in pericarditis), cancer nodes develop, etc. The mechanism by which pericardial friction sounds are generated is similar to that of the pleural friction sounds, except that they depend not on the respiratory movements but on the movements of the heart during systole and diastole. Pericardial friction murmurs vary. Sometimes they resemble pleural friction or the crisping sounds of snow, and sometimes they are very soft, as if produced by rattling of paper or scratching. The following signs can be used to differentiate pericardial friction sounds from intracardiac sounds: (1) there is no complete synchronism of pericardial friction sounds with systole and diastole; friction sounds are often continuous, their intensity increasing during systole or diastole; (2) friction sounds can be heard for short periods during various phases of the heart work, either during systole or during diastole; (3) pericardial friction sounds are not permanent and can reappear at intervals; (4) friction sounds are heard at sites other than the best auscultative points; they are best heard in the areas of absolute cardiac dullness, at the heart base, at the left edge of the sternum in the 3rd and 4th intercostal spaces; their localization is inconstant and migrates even during the course of one day; (5) friction sounds are very poorly transmitted from the site of their generation; (6) the sounds are heard nearer the examiner's ear than endocardial murmurs; (7) friction sounds are intensified if the stethoscope is pressed tighter to the chest and when the patient leans forward, because the pericardium layers come in closer contact with one another.
Pleuropericardial friction murmurs arise in inflammation of the pleura adjacent to the heart and are the result of friction of the pleural layers (synchronous with the heart work). As distinct from pericardial friction sounds, pleuropericardial friction is always heard at the left side of relative cardiac dullness. It usually combines with pleural friction sound and changes its intensity during the respiratory phases: the sound increases during deep inspiration when the lung edge comes in a closer contact with the heart and decreases markedly during expiration, when the lung edge collapses.
Physical and Instrumental Studies of the Vessels
The vessels are studied by inspection, by palpation of arteries and veins, by auscultation of large vessels, and by instrumental examination of the vascular system.
STUDY OF ARTERIAL PULSE
Pulse is the rhythmical vibration of the arterial walls caused by contractions of the heart, blood discharge into the arterial system, and changes in pressure in this system during systole and diastole. Pulse wave is transmit-
ted due to the ability of arterial walls to distend and collapse. The velocity of the pulse wave varies from 4 to 13 m/s, i.e. exceeds significantly the linear velocity of the blood flow, which does not exceed 0.5 m/s even in large arteries.
Palpation of the pulse is the main method of examination of pulse. As a rule, pulse is studied first on the radial artery, since it is superficial and runs immediately under the skin and can thus be readily felt between the styloid process of the radial bone and the tendon of the internal radial muscle. The patient's hand is grasped by the examiner so that the thumb of the right hand is placed on the dorsal side of the arm (near the radiocarpal joint) while the other fingers remain on the frontal side of the arm. As soon as the artery is found, it is pressed against the underlying bone. The pulse wave is felt by the examining fingers as a dilation of the artery. The pulse may be different on different arms, and therefore it should first be palpated simultaneously on both radial arteries. The condition of the vascular wall should be assessed simultaneously. To that end, the artery is pressed by the index and middle fingers of the left hand slightly above the point where the pulse is examined by the right hand. When the vessel stops pulsating under the fingers of the right hand, the arterial wall is felt. A normal artery is a thin elastic tube. In some diseases, for example, in atherosclerosis, the arteries change, their walls become firm, and the course more tortuous. If calcification is considerable, the artery walls are rough, tortuous tubes, sometimes with bead-like thickenings.
Various properties of pulse can be better understood if sphygmograms (pulse curves) are first studied. The diagnostic importance of the pulse will be described later.
Sphygmography. Pulsation of the vascular wall is recorded as a curve (sphygmogram) by an apparatus called sphygmograph. Special pick-ups convert mechanical oscillations of the vascular wall into electric pulses, which are amplified and recorded by an electrocardiograph.
Direct and volumetric sphygmography are distinguished. Direct sphygmography is used to record oscillations of the wall of any superficial artery, for which purpose a funnel is placed on the examined vessel. Volumetric sphygmography records total vibrations of the vascular wall that are converted into vibrations of a portion of the body (usually an extremity). Volumetric sphygmogram is taken by placing a special cuff on the extremity. Curves obtained by direct and volumetric sphygmography do not differ substantially. The distance of the artery from the heart is important for the shape of the pulse curve. Central and peripheral sphygmograms are distinguished accordingly. Central sphygmograms are taken from the carotid and subclavian arteries. Sphygmograms of the radial and femoral arteries, and also volumetric sphygmograms of the extremities are peripheral.
Special Part
Chapter 6. Blood Circulatory System
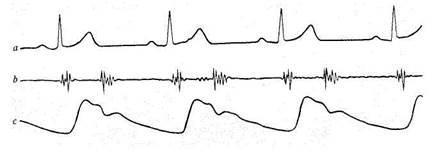
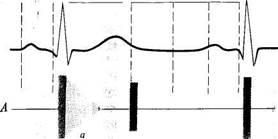
Fig. 36. Normal sphygmogram of the carotid (c) recorded simultaneously with ECG (a) and
PCG (b).
Normal sphygmogram. Both the central and peripheral sphygmograms (Fig. 36) of a healthy individual have a sharp upstroke (the anacrotic wave), a peak of the curve, and a gradually declining downstroke (the catacrotic wave). The catacrotic limb of a peripheral sphygmogram has smaller waves one of which is more pronounced and is known as a dicrotic wave, which is due to repulsion of the blood from the closed aortic valve during early diastole. A central sphygmogram differs from a peripheral one by a pre-anacrotic vibration, a steeper anacrotic wave, a pronounced catacrotic incisura (corresponding to closure of the aortic valve), and a small dicrotic wave. In interpreting a sphygmogram, special attention should be paid to the shape of the pulse waves, the rate of ascent of the anacrotic wave and of descent of the catacrotic wave, the amplitude of the pulse wave, the height of the dicrotic wave, etc.
Properties of arterial pulse. The study of the arterial pulse gives information on the work of the heart and the condition of the circulatory system. The pulse should be taken in the following order. First the examiner must determine if the pulse can be equally felt on both arms. To that end both radial arteries should be palpated simultaneously and the magnitude of pulse waves on both hands compared (normally it is the same). The pulse wave on one arm may happen to be lower. It occurs in unilateral structural abnormalities in peripheral course of the artery, its constriction, compression by a tumour, or a scar, etc. Pulse may also be different when similar changes occur in the brachial or subclavian artery, or due to compression of large arterial trunks by the aortic aneurysm, mediastinal tumour, retrosternal goitre, or markedly enlarged left atrium. The smaller pulse wave may lag in time. If the pulse on the two arms is different, its further study should be carried out on that arm where the pulse
wave is more pronounced. The following properties of pulse are examined: rhythm, rate, tension, filling, size, and form.
Rhythm. In healthy subjects, cardiac contractions and pulse waves follow one another at regular intervals: the pulse is said to be rhythmic or regular. When the cardiac rhythm is upset, pulse waves follow at irregular intervals: the pulse becomes arrhythmic, or irregular. Some pulse waves may be missing or they may appear prematurely, which is characteristic of extrasystole and also complete arrhythmia (fibrillation), in which pulse waves follow one another at irregular intervals.
Pulse rate in normal conditions corresponds to the rate of cardiac contractions and is 60—80 per minute. If the heart rhythm is accelerated (tachycardia), the number of pulse waves increases and the pulse rate increases accordingly (pulsus frequens); slowed cardiac rhythm (bradycardia) is characterized by a respective slowing of the pulse (pulsus rarus). The pulse rate is counted for one minute. If the pulse is arrhythmic, the heart beats should also be counted and compared with the pulse rate. During frequent and irregular contractions of the heart, some systoles of the left ventricle can be so weak that the blood is not ejected into the aorta or the amount of the discharged blood is very small and the pulse wave does not reach the peripheral arteries. The difference between the heart rate and the pulse is called the pulse deficit while the pulse itself is called pulsus defi-ciens. The greater the deficiency, the worse is the effect it produces on the circulation of blood.
Pulse pressure is determined by the force that should be applied to the pulsating artery to compress it completely. This property of pulse depends on the magnitude of the systolic arterial pressure. If arterial pressure is normal, the artery can be compressed by a moderate pressure. A normal pulse is therefore of moderate tension. The higher the pressure, the more difficult it is to compress the artery; such a pulse is called pulsus durus (hard or high-tension pulse). If the arterial pressure is small, the artery is easy to compress and the pulse is soft (pulsus mollis).
Volume of pulse. Pulse volume shows the artery filling with blood, which in turn depends on the amount of blood that is ejected during systole into the arterial system and which produces variations in the artery volume. Pulse volume depends on the stroke volume, on the total amount of circulating blood, and its distribution in the body. If the stroke volume is normal and the artery is sufficiently filled with blood, the pulse is said to be full (pulsus plenus). In abnormal circulation and blood loss, the pulse volume decreases (pulsus vacuus).
Pulse size. The pulse size implies its filling and tension. It depends on the expansion of the artery during systole and on its collapse during diastole. These in turn depend on the pulse volume, fluctuation of the
Special Part
Chapter 6. Blood Circulatory System
arterial pressure during both systole and diastole, and distensibility of the arterial wall. Pulse wave increases with increasing stroke volume, great fluctuations in the arterial pressure, and also with decreasing tone of the arterial wall. This pulse is called large-volume pulse or pulsus magnus. A large-volume pulse is characterized by a high amplitude of pulse fluctuations on a sphygmogram, and it is therefore also called high pulse (pulsus altus). Large-volume or high pulse is characteristic of aortic valve incompetence in thyrotoxicosis, when the pulse wave increases due to the high difference between systolic and diastolic arterial pressure. Such a pulse may develop in fever in connection with decreased tone of the arterial
wall.
Pulse wave decreases with decreasing stroke volume and amplitude of pressure fluctuations during systole and diastole and with increasing tone of the arterial wall. The pulse wave and the pulse become small (pulsus par-vus). Pulse is small when the amount of blood discharged into the arterial system is small, and the rate of its discharge is low. This is observed in stenosis of the aortic orifice or of the left venous orifice, and also in tachycardia and acute cardiac failure. The pulse wave may be quite insignificant (barely perceptible) in shock, acute cardiac failure and massive loss of blood. This pulse is called thready (pulsus filiformis).
In normal conditions, pulse is rhythmic and the pulse wave uniform. Such a pulse is called uniform (pulsus aequalis). In cardiac rhythm disorders, when the heart contracts at irregular intervals, the pulse wave becomes non-uniform, and this pulse is called unequal (pulsus inaequalis). In rare cases (in rhythmic pulse), high and low pulse waves alternate. This is alternating pulse (pulsus alternans). It is believed that this pulse is due to alternation of heart contractions that vary in force. It usually occurs in severe myocardial affection.