
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Increased pressure in the left atrium increases pressure in the pulmonary veins and this in turn causes reflex contraction of the arterioles 4 страница
|
|
Changes
ST and T give one wave (monophase damage potential)
Deep Q. low R, early differentiation of negative T
| Restorative |
Deep Q hoeleciric. V- T negative T (ischaemic)
Cicatrization Deep and broad Q, negative T
Time of appearance
Hfjurs and days from onset of infarction
1-3 weeks from onset of infarction
2- 6 weeks
May remain permanently
Fig. 82. ECG signs of myocardial infarction at its various stages.
Fig. 84. Massive myocardial infarction of the entire anterior wall of the left ventricle, the apex,
and the lateral wall.



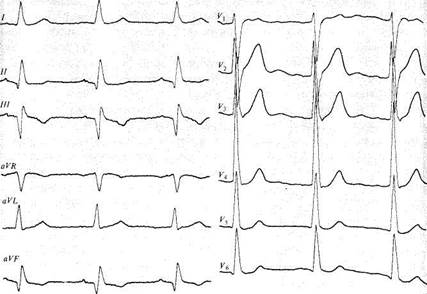
Fig. 83. ECG signs of focal myocardial infarction in the posterior wall of the hypertrophied left ventricle during cicatrization.
In microfocal myocardial infarction. Moderately high temperature usually persists for 1-2 days. Mild leucocytosis is only transient; ESR is slightly increased and the enzymatic activity is increased. The ECG changes are as follows: the S-T segment is below and sometimes above the isoelectric line, and the T wave is either negative or two-phase. These changes disappear in a few days or in a month.
Course. This depends on the size of the affected area, the condition of other arteries of the heart and collateral circulation, on the degree of cardiac and circulatory insufficiency, and on the presence of complications. Cardiorrhexis is among them. It occurs during the first ten days of the disease, during pronounced myomalacia leading to rapid (within a few minutes) death. Fatal outcome may be caused by ventricular fibrillation. Cardiac aneurysm can develop during the disease. An acute aneurysm occurs during the first days of transmural infarction: the increased intraven-tricular blood pressure causes a protrusion at the site of myomalacia of intact layers of the heart wall. The aneurysm is usually formed in the wall of the left ventricle.
The clinical picture of acute cardiac aneurysm is characterized by pericardial pulsation in the 3rd or 4th intercostal space, to the left of the sternum. Auscultation of the heart reveals the gallop rhythm, systolic murmur, and pericardial friction. An acute cardiac aneurysm is
. Special Part
Chapter 6. Blood Circulatory System


 converted into chronic when the necrotized site turns into a scar of connective tissue, or chronic aneurysm can develop at later periods of the disease. Signs of chronic aneurysm are pericardial pulsation, extension of the heart border to the left, systolic murmur in the region of the aneurysm, and a " stabilized" electrocardiogram on which the changes characteristic of acute period of the disease are preserved. X-ray examinations show enlargement of the heart silhouette and paradoxical pulsation. Chronic cardiac aneurysm causes heart failure which is difficult to cure.
converted into chronic when the necrotized site turns into a scar of connective tissue, or chronic aneurysm can develop at later periods of the disease. Signs of chronic aneurysm are pericardial pulsation, extension of the heart border to the left, systolic murmur in the region of the aneurysm, and a " stabilized" electrocardiogram on which the changes characteristic of acute period of the disease are preserved. X-ray examinations show enlargement of the heart silhouette and paradoxical pulsation. Chronic cardiac aneurysm causes heart failure which is difficult to cure.
Cicatrization of uncomplicated myocardial infarction continues for one to three months. The process ends in focal cardiosclerosis.
Treatment. Patients with myocardial infarction are hospitalized during the first hours of the disease. Absolute rest is required. The diet restricted in calories should be free from food that may cause flatulence of the intestine. In the presence of pain attacks, narcotics (morphine hydrochloride and others) are given subcutaneously together with atropine which removes possible side effects such as nausea and vomiting. If narcotics do not help, nitrous oxide mixed with oxygen should be given to inhale through a special anaesthetic apparatus.
In cases with circulatory insufficiency, strophanthin should be given; noradrenaline or mesaton should be given intravenously by a drip method in collapse. Anticoagulants (of direct and then indirect action) should be given during the very first hours of the disease. The duration of hospital stay depends on the gravity of the clinical picture and the degree of the myocardial affection. Spasmolytics and sedatives should be given during the entire disease. Gross transmural, and also recurrent myocardial infarctions should be treated for 3—6 months. The patient often remains disabled.
Cardiosclerosis
Cardiosclerosis (fibroid heart) is the disease of the myocardium caused by developing fibroid elements (cicatrix) in the heart muscle. Atherosclerotic and myocarditic cardioscleroses are distinguished. The latter may result from any myocarditis. Atherosclerotic cardiosclerosis is the result of atherosclerosis of the coronary arteries (diffuse atherosclerotic cardiosclerosis). Myocardial infarction that ends in the formation of scars becomes the cause of focal post-infarction cardiosclerosis.
Clinical picture. The patient complains of decreased work capacity, dyspnoea, first only during heavy exertion, and if the heart muscle is affected considerably, these symptoms appear during usual walk or work. Objective examination of the patient reveals enlargement of the cardiac
dullness to the left. The heart becomes " aortic", its sounds are dulled. Pronounced signs of heart failure may develop later. Cardiosclerosis is the most frequent cause of various arrhythmias such as extrasystole (usually ventricular), atrial fibrillation, or heart block.
Course. Since coronary atherosclerosis tends to progress, cardiosclerosis also becomes more pronounced with time. Myocarditic cardiosclerosis has no progressive tendency.
Treatment. It is the same as that usually given in atherosclerosis, angina pectoris, circulatory insufficiency, and heart arrhythmias.
Chapter 7. Digestive System

 Chapter 7 DIGESTIVE SYSTEM
Chapter 7 DIGESTIVE SYSTEM
OESOPHAGUS
Methods of Examination
Inquiry
Complaints. Dysphagia (difficult passage of food via the oesophagus) is the most frequent symptom of oesophageal pathology. The patient feels difficulty in swallowing (mostly solid food); the food bolus sometimes stops in the oesophagus and the patient feels pain and oesophageal disten-tion. Dysphagia can be due to organic or functional narrowing of the oesophagus. Organic stenosis develops gradually and progresses in cancer, and cicatricial stenosis of the oesophagus. Solid food first passes with difficulty, then the patient feels difficulty in swallowing soft, and then liquid food. When cancer tumour disintegrates, patency of the oesophagus may be restored almost completely. Dysphagia develops immediately in the presence of a foreign body or if the oesophagus is burnt. Dysphagia may also develop due to compression from outside by an aortic aneurysm or mediastinal tumour.
Functional narrowing of the oesophagus is explained by muscular spasms caused by reflex disorders in innervation of the oesophageal muscles, or by neurosis. As distinct from organic dysphagia, functional dysphagia more often occurs in paroxysms when food passes the oesophagus. Sometimes solid food passes more readily than liquid.
Pain occurs in acute inflammation of the oesophageal mucosa (oesophagitis) and in burns. The patient usually feels pain by the course of the entire oesophagus, both with and without swallowing; pain may radiate into the interscapular region.
Patients with achalasia of the cardia (cardiospasm) may have spontaneous attacks of pain, usually during night. Pain is quite severe; it radiates into the back, upwards by the oesophagus, into the neck, the jaws, and continues for minutes and even hours. In the presence of hiatus hernia and gastroesophageal reflux, pain may radiate into the left side of the chest and simulate heart diseases.
Oesophageal vomiting occurs in considerable narrowing of the oesophagus. Food is accumulated over the constricted point, in the wider portion of the oesophagus, and is expelled by antiperistaltic contractions of the muscles. Oesophageal vomiting differs from gastric vomiting in the following: it occurs without nausea and is preceded by the feeling of food
retained behind the sternum; the vomitus includes unaltered (non-digested) food which contains neither hydrochloric acid (gastric juice) nor pepsin; the vomitus containing food that has been taken long time ago has foul odour; taken food can be retained for long periods in the presence of oesophageal diverticulum or degrading cancer.
Regurgitation is the return of swallowed food into the mouth due to oesophageal obstruction. Regurgitation sometimes occurs in neuropathic patients in whom it becomes a habitual symptom or a result of cardiospasm.
Hypersalivation occurs in oesophagitis, cicatricial narrowing of the oesophagus or in cancerous stenosis as a result of the oesophagosalivary reflex.
Afoul breath may be due to a cancer tumour of the oesophagus or congestion and decomposition of food in cardiospasm.
Heartburn (pyrosis) is a specific burning sensation behind the sternum associated with regurgitation of gastric contents into the inferior portion of the oesophagus. This is the cause of the so-called reflux oesophagitis.
Haemorrhage can be due to ulcer of the oesophagus, injury to the oesophagus by a foreign body, degradation of a tumour, bleeding of dilated oesophageal veins (which occurs in congestion of blood in the portal vein system), and also bleeding of the mucosa due to small lacerations of the vessels in the oesophagogastric junction in straining and vomiting (Mallory-Weiss syndrome).
History of present disease. In organic affections of the oesophagus, the disease has a progressive course. Functional diseases (cardiospasm) are characterized by exacerbations connected with psychogenic factors which are followed by remissions. From the anamnesis of the patient's life it can be established whether the patient had past burns of the oesophagus, since acid or alkali burns are frequent causes of cicatricial changes in the oesophagus. Syphilis is an important disease of the past history since the patient's complaints of dysphagia can sometimes be associated with syphilitic aortitis (compression of the oesophagus by a dilated aorta). Development of traction diverticula in the oesophagus may be due to broncho-adenitis in the past (tuberculous broncho-adenitis included). Pul-sion diverticula arise due to oesophagospasm.
Physical Examination
The main objective examination techniques are unimportant for diagnosis of oesophageal pathology. The general inspection of the patient with dysphagia may suggest an organic affection of the oesophagus if the patient is extremely asthenic (cachexia).
 334: Special Part
334: Special Part
Laboratory and Instrumental Methods
Laboratory methods of diagnostication include cytological studies of washings obtained by lavage of the oesophagus with an isotonic sodium chloride solution, or by artificial separation of cells using a bulbous bougie which has rough surface. This procedure should obligatory be done in all cases of suspected newgrowths.
X-ray studies are decisive for diagnosis of oesophageal diseases. Contraindications to X-raying are possible destructive effects of this procedure on the oesophageal wall. Barium sulphate suspensions of various consistency are used as a contrast substance for X-ray examinations. When the suspension is swallowed, the oesophagus becomes visible over its entire length. The oesophageal function can be assessed by observing the passage of the swallowed suspension during roentgenoscopy. X-rays can be used to record separate moments of the oesophagus filling, and also to assess the condition of the oesophageal mucosa. Roentgenocinematography makes it possible to assess peristaltic and contraction ability of the oesophagus. The condition of the oesophageal lumen can be fully assessed only by examining the patient in various positions, e.g. vertical, horizontal, and with the head-end of the bed being thrown back.
The motor function of the oesophagus can be assessed by balloon kymography. Endoscopy with an oesophagofibroscope (a fibre-optic apparatus provided with a device for taking samples of newgrowths protruding into the lumen of the oesophagus) is a valuable diagnostic method. The instrument is very flexible and convenient for endoscopic procedures. Burns of the oesophagus (the first 7-10 days of the disease), corrosive oesophagitis, aortic aneurysm, hypertension (III stage), circulatory insufficiency, and diseases of the larynx are contraindications to oesophagoscopy.