
Главная страница Случайная страница
КАТЕГОРИИ:
АвтомобилиАстрономияБиологияГеографияДом и садДругие языкиДругоеИнформатикаИсторияКультураЛитератураЛогикаМатематикаМедицинаМеталлургияМеханикаОбразованиеОхрана трудаПедагогикаПолитикаПравоПсихологияРелигияРиторикаСоциологияСпортСтроительствоТехнологияТуризмФизикаФилософияФинансыХимияЧерчениеЭкологияЭкономикаЭлектроника
Increased pressure in the left atrium increases pressure in the pulmonary veins and this in turn causes reflex contraction of the arterioles 2 страница
|
|
20*
Special Part
Chapter 6. Blood Circulatory System
of blood from the ventricle to the atrium through an incompletely closed atrioventricular orifice, owing to which pressure increases in the atrium and emptying of the neck and liver veins is made difficult. Tricuspid incompetence is characterized by extensive hepatic pulsation: the liver is displaced anteriorly and swells. This can be felt by trying to hold the liver by both hands: the pulsating liver sets the hands apart during the pulse wave.
Inspection of the patient reveals pronounced pulsation in the region of the right ventricle. As distinct from the heart beat in mitral stenosis, this pulsation is characterized by systolic retraction and diastolic protrusion of the chest.
Systolic retraction of the chest in the region of the right ventricle is explained by pronounced diminution of its volume because much blood is delivered at that moment to the hepatic veins. Systolic retraction of the chest corresponds to the systolic swelling of the liver, and vice versa, diastolic overfilling of the right ventricle and protrusion of the chest in the ventricular region combine with diastolic diminution of the liver volume. Therefore, if the examiner places one hand on the region of the right ventricle and the other hand over the liver, he can feel specific rolling movements of the hands. The apex beat is as a rule not pronounced because the left ventricle is displaced posteriorly by the hypertrophied right ventricle. Percussion reveals marked displacement of the heart border to the right due to hypertrophy of the right atrium and right ventricle.
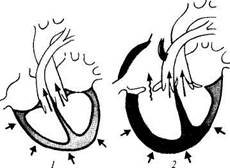
| Wg. 80. Changes in intracardiac haemodynamics in tricuspid incompetence (for designations:, ■;.-• see Fig. 69). |
Auscultation at the base of the xiphoid process reveals diminished first sound; systolic murmur can be heard at the same listening point and also at the 3rd and 4th interspaces, to the right of the sternum; this murmur in-
I
creases when the patient keeps his breath at the height of inspiration. Since pressure in the lesser circulation decreases in tricuspid incompetence, the second sound over the pulmonary trunk decreases in its clearness.
Pulse does not change significantly or it becomes small and fast, because serious heart failure often occurs in tricuspid incompetence. Arterial pressure usually decreases. The venous pressure increases markedly.
Signs of hypertrophy of the right heart's chambers can be detected roentgenographically. Electrocardiography also shows hypertrophy. Phonocardiography records systolic murmur at the base of the xiphoid process and at the 3rd and 4th intercostal spaces, to the right of the sternum; the systolic murmur has a decreasing character. When a phonocar-diogram is taken at the height of inspiration, the vibration amplitude increases.
A phlebogram of the jugular vein reveals a high positive a wave which is connected with the intensified activity of the hypertrophied right atrium, or the wave has the form characteristic of the positive venous pulse.
Echocardiography of the tricuspid valve is more difficult than that of the mitral or the aortic valve. Echocardiograms can reveal paradoxical movements of the interventricular septum in overloading of the right ventricle associated with tricuspid insufficiency.
Tricuspid incompetence usually combines with grave circulatory insufficiency. Long-standing congestion in the greater circulation upsets the function of many organs, such as the liver, kidneys, or the gastro-intestinal tract. The liver is especially affected: prolonged congestion in the liver is attended by growth of connective tissue to provoke the development of the so-called cardiac fibrosis of the liver. This, in turn, even more interferes with the normal function of the organ and causes severe metabolic disorders.
COMBINED AND CONCOMITANT HEART DISEASES
Acquired diseases of the heart, rheumatic in particular, often occur as combined affections of the valves, i.e. valve incompetence and stenosis of the orifice occur simultaneously. Moreover, concomitant affection of two, and sometimes three valves (mitral, aortic, and tricuspid) may occur simultaneously.
Mitral incompetence is most common. It usually concurs with stenosis of the left venous orifice. Signs of both heart diseases are then found but one sign dominates as a rule; less frequently, signs of valvular incompetence and stenosis are equally pronounced.
Dyspnoea and cyanosis are early symptoms of the mitral disease. The
Special Part
Chapter 6. Blood Circulatory System
heart expands to the left, superiorly, and to the right, because both ventricles and the left atrium are hypertrophied. Intensity of the first sound at the apex depends on the prevalent disease: if mitral incompetence is the leading syndrome, the first heart sound diminishes; if mitral stenosis dominates, the first sound increases and becomes squelching. Two sounds are heard at the apex: systolic due to valvular insufficiency, and diastolic due to stenosed orifice.
Pulse and arterial pressure do not change in prevalence of mitral incompetence, while if mitral stenosis dominates, systolic arterial pressure may decrease and diastolic pressure increase; the pulse becomes small.
Combined aortic incompetence is usually secondary to rheumatic endocarditis. Both systolic and diastolic murmurs are characteristic; these sounds can be heard over the aorta. Vascular pulsation and high pulse pressure are typical of aortic incompetence; they are not so pronounced in combined aortic affection. At the same time, slow and small pulse, and low pulse pressure that are typical of aortic stenosis, are also less pronounced in combined aortic incompetence.
Detailed clinico-instrumental examination of patients with concomitant affections of several valves reveals signs typical of each particular disease. It is necessary in such cases to conclude on the gravity of each disease and the prevalence of one of them. This is especially important for prognostic conclusions and for prospective surgical treatment.
Prognosis and treatment of heart diseases. The course of heart diseases and their prognosis depend on many factors. Mild changes in the heart valves, in the absence of marked affections of the myocardium, can remain non-manifest for a long time without impairing the work capacity of the patient. Aortic insufficiency is compensated for a long time but when decompensation develops, the patient soon dies. Mitral stenosis has a worse prognosis because the disease is compensated by a weaker left atrium. Congestion soon develops in the lesser circulation, which is followed by incompetence of the right heart chambers, and the greater circulation soon becomes affected by congestion. Repeated rheumatic attacks have an adverse effect on the course of the disease: the valvular apparatus of the heart is progressively impaired and the myocardium is affected. These disorders provoke circulatory insufficiency. Moreover, any infection, poisoning, physical or nervous overstrain, pregnancy and labour may give an impetus to the development of heart failure.
Restitution prognosis depends on the general condition and physical fitness of the patient. In the absence of symptoms of circulatory insufficiency, the patient may return to his usual occupation; in the presence of signs of decompensation, the patient should be recommended to change his occupation. Work capacity can be preserved in a patient with heart disease
provided he fulfills special recommendations for his work and rest, if he abstains from overeating, smoking, or drinking. Remedial exercises can be prescribed to strengthen the myocardium in the absence of cardiac insufficiency.
Prophylaxis of heart diseases consists mainly in prevention of rheumatism, sepsis and syphilis. Prophylaxis also implies sanation of infectious foci, strengthening of the body, and exercises.
Conservative treatment of patients with heart diseases consists in prophylaxis and treatment of heart failure. Mitral stenosis is often corrected surgically (mitral comissurotomy). The adhered cusps are disjoined and the atrioventricular orifice is widened. This operation removes severe haemodynamic disorders. Aortic comissurotomy is performed in stenosed aortic orifice, but this operation is much more complicated. Surgical treatment of mitral and aortic incompetence consists in replacement of the destroyed valve by an artificial one.
Patients with rheumatic heart disease should be regularly observed in out-patient conditions.
Myocarditis
Myocarditis is inflammation of the myocardium. The disease affects both men and women at any age. Acute, subacute, and chronic myocarditis are differentiated. The disease may be local or diffuse.
Aetiology and pathogenesis. Aetiological factors responsible for the development of myocarditis are various bacterial and virus infections. The most common cause of myocarditis is rheumatism, next come sepsis, diphtheria, rickettsiosis, scarlet fever, and virus infections. Myocarditis may develop in sensitization to some medicinal preparations (allergic myocarditis). Inflammatory changes in the myocardium caused by various infections are the result of allergic reaction of the body sensitized by certain microbes. The microbe antigen or its toxin act on the myocardium to cause formation of tissue antigens (auto-antigens) in it. As a result, auto-antibodies are formed which account for the vast changes in the myocardium.
Pathological anatomy. Dystrophic processes in the muscle fibres are characteristic. Predominant exudative or proliferative processes are also observed in the interstitial tissue (interstitial myocarditis). The outcome of the inflammatory changes is cardiosclerosis.
Clinical picture. This includes signs of decreased contractility of the myocardium and upset cardiac rhythm. The patient complains of dyspnoea in physical exertion, extreme weakness, palpitation, intermissions, dull and boring pain, or attacks of pain in the heart (like in angina pectoris).
Special Part
Chapter 6. Blood Circulatory System



 The skin is pallid, sometimes with a slight cyanotic shade. In pronounced heart failure the neck veins become swollen. The pulse is small, soft, sometimes arrhythmical and accelerated: it may however be slowed down too. Extrasystole and, less frequently, paroxysmal fibrillation develop in deranged excitation function and automaticity.
The skin is pallid, sometimes with a slight cyanotic shade. In pronounced heart failure the neck veins become swollen. The pulse is small, soft, sometimes arrhythmical and accelerated: it may however be slowed down too. Extrasystole and, less frequently, paroxysmal fibrillation develop in deranged excitation function and automaticity.
Decreased diffuse apex beat, which is displaced anteriorly, is revealed on examination of the heart. Percussion can detect displacement of the heart to the left. Auscultation reveals a markedly decreased first sound at the early systole (due to decreased rate of rise in the intraventricular pressure). The second sound is either unchanged or diminished due to hypotension. Gallop rhythm can be heard in significantly decreased myocardial contractility. Systolic murmur can often be heard over the heart apex. It arises due to relative mitral incompetence. Arterial pressure, especially systolic, decreases and the pulse pressure falls accordingly.
ECG changes in myocarditis are quite varied and transient. Sinus tachycardia, sinus arrhythmia, and extrasystole (in the form of separate or group atrial or ventricular extrasystoles) can most frequently be found on electrocardiograms. Conduction is deranged according to incomplete or complete atrioventricular block. Diffuse affections of the myocardium are shown on ECG as diminished and split P wave, changed QRS complex (decreased voltage of the waves and their splitting), decreased S-T interval, the presence of two phases and inversion of the decreased T wave.
The blood counts show moderate neutrophilic leucocytosis with shift to the left, increased ESR, and hyperglobulinaemia (mainly due to a2- and 7-globulins).
Course. The course of myocarditis is usually favourable and ends with recovery. Sclerosis of the myocardium develops in some patients (myocardial cardiosclerosis).
Treatment. Myocarditis patients are prescribed strict bed-rest. The main cause that provokes the disease is treated by antibiotics, desensitizing preparations, and hormones. Cardiac glycosides and diuretics are given in the presence of heart failure. In order to improve metabolism in the myocardium, carboxylase, ATP, vitamins, and potassium preparations are prescribed. Deranged cardiac rhythm can be restored by appropriate preparations.
Cardiomyopathy
Cardiomyopathy includes diseases of unknown aetiology characterized by affections of the heart muscle attended by enlargement of the heart and its insufficiency.
The following three types of cardiomyopathy would be usually dif-
ferentiated: (1) congestive or dilatation; (2) hypertrophic; and (3) restrictive cardiomyopathy.
Congestive cardiomyopathy is characterized by dilatation of the heart chambers with pronounced heart failure. The patients develop dyspnoea during slightest physical exertion and even at rest, attacks of suffocation and cardiac pain which cannot be removed by nitroglycerin; heart palpitation and intermissions are also characteristic. As circulatory insufficiency progresses, the liver becomes.enlarged and oedema and hydrops of the cavities develop. The borders of the heart are markedly displaced to the right, upwards, and to the left. The heart sounds at the apex are dulled, the second sound over the pulmonary trunk is accentuated, gallop rhythm often develops along with systolic murmur at the apex due to developing relative mitral insufficiency. The pulse is small and fast, sometimes arrhythmical. The arterial pressure is usually decreased.
ECG in congestive cardiomyopathy shows various changes in the myocardium; signs of overloading of the heart chambers and focal changes develop along with rhythm and conduction disorders.
Echocardiography reveals marked dilatation of the heart chambers and decreased contractility of the myocardium.
Hypertrophic cardiomyopathy is characterized by the primary hypertrophy of the myocardium with subsequently developing cardiac insufficiency which differs but little from congestive cardiomyopathy by its symptoms.
The special form of hypertrophic cardiomyopathy is obstructive cardiomyopathy, which is also known as idiopathic hypertrophic subaortic stenosis. This cardiomyopathy is characterized by asymmetric hypertrophy of the interventricular septum in the region of blood outflow from the left ventricle. The cavity of the left ventricle diminishes. A circular ridge of the hypertrophied myocardium is formed beneath the aortic valve. The ridge interferes with blood ejection into the aorta. This form of myocardiopathy is first manifested by symptoms characteristic for aortic stenosis: the patient develops headache, giddiness, faints, and heart pain (like in angina pectoris). Palpation and percussion of the heart reveals hypertrophy of the left ventricle; auscultation reveals coarse systolic murmur which is best heard at the 3rd or 4th intercostal space at the left edge of the sternum. The pulse is small and slow. Symptoms of circulatory insufficiency soon appear.
Echocardiography is most important among additional methods used to diagnose hypertrophic subaortic stenosis. It reveals asymmetrical hypertrophy of the interventricular septum, narrowing of the left ventricle and systolic deflection of the mitral valve cusp in the direction of the interventricular septum.
Special Part
Chapter 6. Blood Circulatory System 315


 Hypertrophic cardiomyopathy can be familial, inherited by the autosome-dominant type.
Hypertrophic cardiomyopathy can be familial, inherited by the autosome-dominant type.
Restrictive cardiomyopathy is associated with disordered distensibility of the myocardium due to endocardial and subendocardial fibrosis. The diastolic function of the myocardium becomes upset and heart failure (without marked hypertrophy of the myocardium or dilatation of the heart chambers) develops.
Pericarditis
Pericarditis is inflammation of the pericardium.
Aetiology and pathogenesis. In most cases pericarditis develops in the presence of rheumatism or tuberculosis. Rheumatic pericarditis usually concurs with affection of the myocardium and endocardium. Rheumatic, and mostly tuberculous pericarditis are manifestations of infectious allergic process. In certain cases, tuberculous pericarditis depends on the spread of infection from the foci in the lungs and tracheobronchial lymph nodes (via the lymph ducts to the pericardium). Pericarditis can develop in other infections as well (e.g. scarlet fever, measles, influenza, or sepsis). Sometimes it develops due to the transition of inflammation from the adjacent organs in pleurisy, pneumonia, myocardial infarction, and also in injuries to the heart and in uraemia.
Pathological anatomy. Dry (fibrinous) pericarditis and pericarditis with effusion are distinguished. Depending on the character of effusion, pericarditis may be serous, serofibrinous, purulent, or haemorrhagic. Serous effusion and small masses of fibrinous ex-udate may be fully resorbed. Fibrinous and purulent effusions undergo organization to thicken the pericardium membranes and cause commissures. Pericardium layers sometimes become adherent and the pericardial sac disappears (concretio pericardii). This condition is known as adherent (adhesive) pericarditis. Calcium is often deposited in the affected pericardium and the heart becomes enclosed in a rigid case. The dense fibrous thickening of the pericardium compresses the heart. This condition is known as constrictive pericarditis.
DRY PERICARDITIS
Clinical picture. Pain in the heart is often the only complaint of patients with dry pericarditis. The pain varies in character from discomfort and pressure to strong torturing pain with radiation to the left part of the neck and the shoulder blade.
Inspection and percussion of the heart do not reveal any changes unless myocarditis or other heart diseases concur. The most important, and sometimes the only sign of dry pericarditis is the sound of pericardial friction. Dry pericarditis ends with complete recovery in 2—3 weeks; or the disease may convert into pericarditis with effusion or adhesive pericarditis.
. PERICARDITIS WITH EFFUSION
Clinical picture. Patients complain of the pressing sensation in the chest and pain in the heart. As effusion is accumulated, dyspnoea develops. Dysphagia develops in compression of the oesophagus and hiccup when the phrenic nerve is compressed. Fever is an almost obligatory symptom.
The appearance of the patient is characteristic: the face is oedematous and the skin is cyanotic and pallid. The neck veins are swollen due to an obstructed blood flow to the heart via the superior vena cava. Compression of this vein accounts for the oedematous appearance of the face, neck, and the anterior surface of the chest (Stokes' collar). The neck veins may sometimes swell only during expiration. If much exudate is collected in the pericardial sac, the patient assumes a characteristic posture: he sits in bed and inclines forward, his hands resting against the pillow lying on his knees. The feeling of heaviness in the heart is thus lessened and respiration made easier.
Inspection of the heart region reveals levelling of the interspaces. The apex beat is absent; if it is palpable, it appears to be displaced superiorly or medially of the left border. Percussion shows considerable enlargement of the cardiac dullness in all directions, absolute and relative dullness being almost undistinguishable. The area of dullness resembles a trapezium or a triangle: the right cardiohepatic angle becomes obtuse. If much exudate is accumulated, dullness extends to the left to diminish the tympany zone of Traube's space. Heart sounds are markedly decreased. The pulse is accelerated, small, and sometimes paradoxical. Arterial pressure is normal or decreased. Venous pressure is elevated. Palpation of the abdomen reveals marked enlargement of the liver due to congestion of blood in it. X-ray study shows enlarged heart silhouette in the transverse direction and superiorly; the waste of the heart is absent, the pulsation is markedly weak, which is especially vivid on the X-ray picture.
The ECG shows low voltage of all waves and also changes in the S-T interval and the T wave in all standard leads. The S-T interval is first located above the isoelectric line and then below it. The T wave is first low and then becomes negative. The ECG changes are like those observed in myocardial infarction except that they are equally pronounced in all leads (concordant), and that the Q wave remains unchanged.
Echocardiography is very important in the diagnosis of pericarditis with effusion. Echocardiography reveals the space between the pericardium and epicardium which is filled with fluid that does not return the probing ultrasound pulses. If effusion is small, the echo-free space can only be revealed between the pericardium and the posterior wall of the heart in a
Special Part
Chapter 6. Blood Circulatory System
 patient in the supine position. In the presence of a large effusion, this space can be revealed in the region of the anterior wall of the heart.
patient in the supine position. In the presence of a large effusion, this space can be revealed in the region of the anterior wall of the heart.
Course. Purulent pericarditis is a grave danger to the patient's life unless urgent treatment is given. Serous pericarditis may end in complete recovery. Adhesive pericarditis produces persistent pathology because operative separation of the pleural layers is not sufficiently effective.
Treatment. Treatment depends on the cause of pathology. Rheumatic pericarditis is treated as rheumatism, and tuberculous pericarditis as tuberculosis. Various cardiacs and stimulants should be given in the presence of cardiac insufficiency. If effusion is large, the pericardium is punctured and the fluid withdrawn.
Essential Hypertension
Essential hypertension (morbus hypertonicus) is the condition in which elevated arterial pressure is the leading symptom. The disease is provoked by nervous and functional disorders in the regulation of the vascular tone. Men and women, mostly over 40, are equally attacked by the disease.
Essential hypertension should accurately be differentiated from symptomatic hypertension in which arterial pressure rises as a symptom of some other disease, this symptom being far from the leading one. Symptomatic hypertension occurs in aortic coarctation, atherosclerosis of the aorta and its large branches, in endocrine dysfunction (e.g. Itsenko-Cushing disease, phaeochromocytoma, primary aldosteronism, or the Conn syndrome), affection of the renal parenchyma, occlusive affection of the main renal arteries, and in some other diseases.
Aetiology and pathogenesis. Overstrain of the central nervous system, caused by prolonged and strong emotional stress and also mental overstrain, are believed to be the main cause of the disease. In some cases essential hypertension develops after brain concussion (concussion-commotion form). The importance of neurogenic factors was emphasized by Lang in 1922; later this hypothesis was confirmed by the Soviet physicians during World War II: the incidence of essential hypertension increased significantly in the sieged Leningrad.
Development of the disease greatly depends on occupation: it occurs mostly in subjects whose occupation is associated with nervous and mental overstrain, e.g. in scientific workers, engineers, physicians, drivers, etc. Familial predispostion is another important factor.
The early stage of essential hypertension is characterized by nervous-functional disorder in regulation of the vascular tone. Vegetative-endocrine disorders and changes in the renal regulation of the vascular tone are later steps of the pathological process. Overstrain of the higher nervous
activity causes vasopressor adrenal reaction by which arterioles, mainly the arterioles of the internal organs and especially of the kidneys, are narrowed. Ischaemia of the renal tissue develops as a result. This in turn stimulates production of renin by the juxtaglomerular cells of the kidneys. Renin stimulates formation of angiotensin-II which in turn causes a pronounced pressor effect and stimulates secretion of aldosterone (sodium-retaining hormone) by the adrenal cortex. Aldosterone promotes transition of sodium from the extracellular fluid into the intracellular fluid to increase the sodium content of the vascular wall. This causes oedematous swelling of the wall and narrowing of the vessel, which in turn promotes elevation of arterial pressure.
There is a system of depressor factors in the body whose dysfunction plays an important role in the pathogenesis of essential hypertension. Bradykinin and angiotensin, which produce a depressive effect, have been isolated. It is believed that the depressor system becomes altered by some unknown reason during essential hypertension.
Pathological anatomy. Essential hypertension gradually affects permeability of vascular walls and their protein content. At late or grave forms of the disease, this causes sclerosis or necrosis of small arteries and secondary changes in the tissues of organs. Walls of large vessels are usually affected by atherosclerotic changes. The extent of vascular affection differs in various organs and various clinicoanatomical variants of the disease therefore arise, with a prevalent affection of the vessels of the heart, brain, or kidneys (primary cirrhosis of the kidneys thus develops).
Clinical picture. During the early stage of the disease, the patient would usually complain of neurotic disorders: general weakness, impaired work capacity, inability to concentrate during work, deranged sleep, transient headache, a feeling of heaviness in the head, vertigo, noise in the ears, and sometimes palpitation. Exertional dyspnoea (ascending upstairs, running) develops later.
The main objective sign of the disease is elevated systolic pressure (over 140-160 mm Hg) and diastolic pressure (over 90 mm Hg). Arterial pressure is very liable during the early stage of the disease, but later it stabilizes. Examination of the heart reveals signs of hypertrophy of the left ventricle: expanding apex beat, and displacement of the cardiac dullness to the left. The second sound is accentuated over the aorta. The/ pulse becomes firm and tense.
X-rays reveal " aortic" silhouette of the heart. The aorta is elongated, consolidated, and dilated.
The ECG is of the left type with displaced S-T segment, low, negative, or two-phase T wave in the 1st and 2nd standard chest leads (V5-Vg).
Coronary atherosclerosis concurs not infrequently. This may cause angina pectoris and myocardial infarction. In the late period of the disease,
Special Part
Chapter 6. Blood Circulatory System
 heart failure may develop due to fatigue of the heart muscle as a result of increased arterial pressure. Heart failure is often manifested by acute attacks of cardiac asthma or oedema of the lungs; or chronic circulatory insufficiency may develop.
heart failure may develop due to fatigue of the heart muscle as a result of increased arterial pressure. Heart failure is often manifested by acute attacks of cardiac asthma or oedema of the lungs; or chronic circulatory insufficiency may develop.
Vision may be deteriorated in grave cases. Examination of the fundus oculi reveals its general pallidness; the arteries are narrow and tortuous, the veins are mildly dilated; haemorrhage into the retina (angiospastic retinitis) is sometimes observed.
High arterial pressure in the affected cerebral vessels can derange cerebral circulation. This can cause paralysis, disorders in sensitivity, and sometimes death of the patient. Cerebral circulation is deranged due to spasms of the vessels, their thrombotic obstruction, haemorrhage due to rupture of the vessel, or diapedetic discharge of erythrocytes.
The affected kidneys become unable to concentrate urine (nicturia or isohyposthenuria develops). Metabolites (otherwise excreted with urine) are retained to provoke uraemia.